

Judith's Blog
Judith's Blog
Judith's Blog
Judith's Blog
Judith's Blog
Judith's Blog

New subspecialties are evolving in the caregiving and management space. Preplanning is always preferable to addressing needs during a crisis or at the time of a loss. Aging individuals and those with chronic illnesses are prime candidates. They need to express their preferences for care when they can, so others are unable to do so. It is important that they also explore options to assist their loved ones in navigating after they pass. A resource to consider is an after-loss professional. My interview with Abby O’Leary, the founder of Fare Well Associates, sheds light on a wonderful emerging resource.
What is an after-loss professional?
I like to think of myself as a concierge and project manager for individuals and families dealing with the loss of a loved one. There are so many administrative and logistical questions that surface after a death. These include working with funeral homes, dealing with personal possessions, coordinating with attorneys and accountants, and closing accounts and subscriptions. I help my clients identify all those to-do’s, put together a plan, and cross things off the list.
What prompted you to start Fare Well Associates?
When my father died less than a month after being diagnosed with cancer in 2021, I was shocked at how much there was to do while grieving. Within just the first several weeks, I had to contact over 30 institutions to begin wrapping up his affairs. This process took months. By the end, I learned so much (the hard way), and I saw a real opportunity to share that expertise with others.
What are the most common issues your clients face?
After the loss of a loved one, there are so many decisions to be made and actions to take. Unfortunately, this is a time when folks have little capacity to deal with it all. Grief, shock, and numbness can make it difficult to tackle seemingly mundane tasks, especially when those tasks turn out to be more complicated than expected. For example, closing or transitioning a bank account is a very common to do item. It is not as simple as a quick phone call and may require multiple follow-ups. It can feel like herding cats, and when you’re grieving, it’s too much to shoulder on your own.
When should someone contact an after-loss professional?
I work with families who may be anticipating a loss due to illness or have recently lost a loved one. When the sense of being overwhelmed and frustration build it’s time to reach out for assistance. The earlier the better!
Are there steps people can take in advance to make after-loss easier for their loved ones?
Absolutely! People often say, “We’re all set, we have our will done,” that’s a necessary first step, it’s just the first step. Organizing your important documents, and account information, and writing your wishes for possessions and valuables are additional steps. Talking to your family members to ensure they have the necessary information is key to having them follow your wishes. In addition to the after-loss work I do, I also offer Advance Planning “End of Life Audits”. Clients are often surprised at just how much additional information still needs to be gathered.
What should someone look for when considering an after-loss professional?
After-loss is an emerging field. A great starting place is to check out the directory offered by Professionals of After Loss Services. This association is dedicated to training and community-building within our profession. Most of us provide a free discovery or informational call. You can use that as an opportunity to ask somebody about their experience, their methods, and their pricing. And above all, trust is key. After-loss professionals are not your attorneys or financial advisors. It’s likely that you’ll be sharing sensitive and personal information during the process. Be sure that the person you’re working with has a solid commitment to confidentiality and data security.
Biography and Contact Info
Fare Well Associates founder Abby O’Leary came face-to-face with the bureaucracy of death when her father died less than a month after being diagnosed with metastatic melanoma in early 2021. She saw a huge gap in the support available to families dealing with it. In response, she founded Fare Well Associates. She offers customized planning, organization, and project management services for individuals and families dealing with loss.

Abby O’Leary abby@farewellassociates.com 919-307-1526 www.farewellassociates.com

Empowering People to Be Their Own Best Advocate When Entering the Healthcare System
The Healthcare system is like no other service we use in our daily lives. The Healthcare system is complex, fragmented, costly, and can be dangerous. Most of us were never trained in how to use the healthcare system so it works for us when we need it. Learn how patients and their families can be their own best advocates when navigating the complex healthcare system.
Why Families Need Empowerment
The question of why patients and families need empowerment surfaces frequently. Consider the complexity of the US health system and your ability to navigate it. Challenges like health status, age, income, employment status, insurance coverage options, and provider availability in your area are some of the things that can impact your ability to access healthcare. For those with chronic, catastrophic, or overwhelming medical or mental health conditions, one’s ability to manage their or their family’s care can be overwhelming. People need to be empowered to navigate the complex healthcare system.
Decision Making: Being the Best Advocate
When one is sick and focusing on their illness, they may not have the ability to think beyond their immediate needs and the consequences of decisions being made. Knowing the questions to ask and advocating for needed and covered medical services takes knowledge, initiative, resourcefulness, and accountability. Making the wrong decision or not acting in a timely manner can have a significant burden on your health as well as your finances.

Practical Advocacy Tips
- Get a notebook to keep important information about your doctors; their names, phone numbers, and dates of your appointments
- Keep track of any testing you are asked to have done. Note the type of test, the date, and the results
- Keep a medication list; include all supplements and herbal preparations. Write the name of the drug, the dose and how often you take each medication, and the reason it’s being taken. For example, diabetes, heart disease, or an infection. Note if you have any reactions from the drug.
- Take notes when you talk to any medical professional or your insurance company. Write the date of the call/conversation, who was present, and what was said. Is there any follow-up you must do? Note if there is any follow-up the person you are talking to you has to do. If there is any follow-up, put a note on your calendar for the date the follow-up is due. This will remind you to check to see what your test or lab work found. Don’t ‘assume’ someone will follow up. If you don’t hear anything, take the initiative to follow up yourself.
- Explore the use of various digital apps for helping you communicate with the care team, remind you to order or take medications, track your Advance Directive, or manage your condition.
Not all insurance is the same!
People need to understand their insurance coverage. Take time to review your policy so you understand your insurance coverage. As each policy is different you need to know about your policy. When you get new insurance, ask for a member handbook. The member handbook explains what your policy covers and what it does not cover. There will also be information on exclusion periods, deductibles, out-of-network, co-pays, and pre-existing conditions which may result in barriers to accessing much-needed medical care.
Depending on one’s insurance coverage you may not be entitled to all the care and services needed. Out-of-pocket expenses also vary based on insurance coverage. In some circumstances, your doctor or specialist can write a letter with details as to why you need a test, equipment, or extra time in the hospital. This information is valuable and gives your insurance company the information they need to approve the request or make an exception to the policy.
Being an active member of your team allows you to ask questions, so you understand everything that is happening. By understanding your diagnosis and plan of care you will have a vested interest in helping the plan will work.
Resources for Empowering
Ask Me 3: Good Questions for Your Good Health
Judith and Anne will provide more tips to empower you to be your own best advocate, so you get the care you need when you need it at the right time and in the least restrictive setting.
If you have any topics, you would like us to cover, please put your request in the comment section and we will address them in a future post.
Thanks,
Judith & Anne

The bathroom is one of the most dangerous rooms in a residence, where many accidents can happen. Addressing bathroom safety is key to minimizing injuries. Bathroom accidents can range from slips and falls to burns, electric shocks, poisoning, and drowning. Therefore, it is important to follow some bathroom safety tips to prevent injuries and ensure the well-being of yourself and your family.
Bathroom Safety Tips
Tub Safety to Minimize Injuries
We are often reminded never to leave a small child unattended in the bath. Children can drown in just a few inches of water, always supervise them and have all the supplies handy before bath time. Do not rely on bath seats, swim rings, or other devices to keep children safe.

Avoid the danger of scalding. Water that is too hot can cause serious burns, especially for children and older adults who have more sensitive skin. Turn down the temperature of your water heater to below 120°F (49°C) and always check the water temperature before getting into the tub or shower. Consider installing anti-scald devices or digital faucets that regulate the water temperature. Bathroom Safety is Key to Minimizing Injuries, a small upfront investment may avert a crisis.
Grab Bars to Minimize Injuries
Install grab bars in the shower, tub, and toilet areas. Grab bars can help you maintain your balance and prevent falls when getting in and out of the shower or tub, or when using the toilet. They should be installed either vertically or horizontally, not diagonally, and be sturdy enough to support your weight. Towel rails are not a good substitute for grab bars.

Slip Prevention is Vital to Minimizing Injuries
Reduce the risk of slipping. Wet floors, rugs, and tubs can be very slippery and cause falls. Utilize non-skid strips or mats to the tub bottom and use slip-resistant rugs or mats outside the tub. Remove these rugs once you are dry so that they do not become a trip hazard. Dry wet floors as quickly as possible and avoid wearing socks or shoes that can slide on wet surfaces.
Toilet Dangers
Always close and lock the toilet lid. This can prevent small children from falling into the toilet and drowning, or from accessing harmful substances that may be in the toilet bowl or tank. You can also use a toilet lock that has an automatic reset function to make it easier for adults. Closing the toilet lid when flushing; minimizes the spread of vapor particles that carry bacteria and other pathogens to spray around the bathroom.

Storage- Often Overlooked in Bathroom Safety
Appropriate medication and cleaning product storage. Medications and cleaning products can be poisonous if ingested or misused by children or adults. You should keep them in clearly marked containers, either in their original packaging or in a special pill dispenser, and store them out of the reach of children in a locked cabinet away from everyday items such as shampoo, soap, etc. Avoid using toxic chemicals for cleaning and opt for non-toxic green alternatives whenever possible. Many medications are damaged and lose their potency by the heat and moisture of the bathroom. Avoid storing them in the bathroom medicine cabinet.
Electrical Safety
Safeguard against electric shock. Electricity and water do not mix well and can cause fatal shocks if they come into contact. You should install GFCI (ground-fault circuit interrupter) outlets in your bathroom to protect against electric surges and hire an electrician to do this job for you. You should also avoid using electrical appliances such as hair dryers, curling irons, or radios near water sources or wet surfaces. Remember that hot curling irons and straighteners remain hot for a while; keep them out of the reach of children and those with dementia.
Ensure lighting is adequate and shadows are limited. Utilize night lights that turn on automatically in the dark and avoid the use of extension cords.

Conclusion
Bathroom Safety is Key to Minimizing Injuries! You can reduce the risk of accidents and injuries in your bathroom and make it a safer place for yourself and your family
- Critically review your bathroom for lurking hazards.
- Consider utilizing the services of an occupational therapist or a contractor specializing in bathroom modifications.
- Implement these bathroom safety tips
- Remember that Bathroom Safety is Key to Minimizing Injuries. Injury prevention is better than managing a crisis. Safety is more important than aesthetics.
Stay safe in your bathroom!
Resources:
Spring Cleaning and Fall Prevention
CDC Report Shows Bathroom Injuries Cause Thousands of Visits to ER
Consumer-Focused Education from Judith and Anne; Two Nurses Who Have Seen It All!
Two Nurses Who Have Seen It All!
Judith Sands, RN, MSL, BSN, CPHRM, CPHQ, CCM, ARM, and Anne Llewellyn, RN-BC, MS, BHSA, CCM, CRRN, BCPA, CMF are two nurses who have seen it all! They have been colleagues and friends since the late 80s and have kept in touch over the years. Each time they connect, they have stimulating conversations about the complexity of the healthcare system, and the challenges people have navigating it. These two advanced practice nurses want to help PEOPLE, (patients and caregivers) navigate the complex healthcare system. So people get the care they need when they need it in an efficient way to meet THEIR needs. Judith and Anne work to assist the care team in delivering safe, quality, cost-effective care.
Recently, they talked about putting together a series to share information to educate and empower individuals to be their own best advocates. Judith and Anne want to provide the just-in-time and pre-planning information. The goal is to facilitate better management of illness, caregiving navigation, and minimize complications in the process. Get to know Jusith and Anne, they will be moving into various mediums where they will take questions and interact with those seeking guidance.
Get to know Judith and Anne
Judith Sands
Judith Sands is a wife, mother, grandmother, friend, and caregiver who assumed this role on several occasions for family members. Originally from Buffalo, NY, she spent the majority of her professional career in South Florida. A registered nurse for over 40 years and practiced critical care before specializing in quality, risk, and case management. As a director of case management, she worked closely with her team and families on discharge planning/continuity of care, end-of-life, and where to find resources and support for those with limited funds.
Judith authored Home Hospice Navigation: The Caregiver’s Guide. The book was a response to her mother’s question “What do people do if they don’t have someone like you?” It is filled with tips that can help address advanced care planning and caregiving approaches before a crisis or major change in condition occurs. Knowing your loved one’s wishes and being able to honor them helps guide the caregiving journey.
Anne Llewellyn
Anne Llewellyn is a wife, sister, friend, nurse, and Brain Cancer Survivor. She grew up in Philadelphia PA and moved to Florida when she married. A nurse for 50 years, starting as a licensed practice nurse and advancing to a registered nurse where she practiced critical care (Emergency Department and Respiratory Intensive Care). She specialized in case management, rose through the ranks, and served in the role of president of the Case Management Society of America.
Anne worked as a catastrophic case manager and specialized in group health, workers’ compensation, long-term care, and continuing education. In 2014 her life changed when she was diagnosed with a Brain Tumor. She realized for the first time how hard it is to be a patient. As she progressed on her journey, Anne promised once she recovered and could go back to work, she transitioned her career into nurse advocacy to help people to learn how to be their own best advocates. Today she works directly with people to assist them with care coordination, transitions of care, and self-advocacy. She provides education in her community and through various social media sites.
Both Judith and Anne love to travel, swim, read, and visit family and friends.
Thank you for taking the time to hear about Judith and Anne. Let them know what questions you have and topics you would like to see addressed. They will be back with more articles to empower you! Stay Tuned!
Resources:
You can reach out to:

Judith at Judith@JudithSands.com, Visit JudithSands.com

Anne at allewellyn48@gmail.com
Visit Nurses Advocates

Caregiver, are you suffering from “Fudge”? It’s a rhetorical question. Caregiving is one of the most demanding jobs there is and most don’t even know that they are suffering from “Fudge”. Describe any caregiver that you have seen and no doubt you will know that they were suffering from some or all of the “Fudge” symptoms. Every caregiver suffers from “Fudge” to varying degrees given the nature of the support provided and the duration of caregiving. The degree of “Fudge” suffered will fluctuate based on the care demands and the status of the caregiver at that moment.
What is “Fudge”?
“Fudge” is an acronym for Frustrated, Unsure, Guilty, Depressed, and Exhausted. These are the key symptoms that affect caregivers.
Frustration is the most common sentiment expressed by caregivers. The issues leading to caregiver frustration include the ongoing changes in the needs of the one being cared for. Just when a routine is mastered, things happen, and the status quo is blown away. Providers and vendors who don’t turn up when scheduled and supplies that don’t arrive when expected contribute to pushing the caregiver to the limits.
Unsure; what happens now? When a new symptom is exhibited, an unexpected reaction surfaces or there is an unplanned turn of events, that often results in a caregiver doubting their abilities. They lack confidence and are uncertain as to what actions should be taken. Frequently, this happens late at night, on weekends, or on holidays when support is limited.
Depression is the sadness and despair that accompanies caregiving. It is magnified as the loved one’s condition declines and care needs increase. Caregivers become more sleep deprived, and they may also experience a loss of social support. If the caregiver has a history of depression, then symptoms are magnified.
Guilty feelings surface when a caregiver is stressed by growing caregiving needs. There is a realization that they may no longer be able to provide care, or they are “sandwiched” between caring for others (child, grandchild beyond caring for a spouse) or they need medical interventions.
Exhausted, the caregiver is suffering from physical and or mental tiredness. The caregiver experiences difficulty concentrating and encounters sleep issues. Sadly given all that they are dealing with caregivers tend to disconnect from relationships and support mechanisms. FUDGE is another way to describe caregiver burnout.

Reduce your “Fudge”
Caregiver, are you suffering from “Fudge”? A question that needs to be continually asked. Managing “Fudge” is an active and ongoing process. The caregiver must practice self-care to ensure that they can continue effective caregiving responsibilities. Just as passengers on a flight are reminded that in the event of the loss of cabin pressure and oxygen masks are deployed, one is instructed to place their mask on first before helping others.
Consider what you could realistically delegate; shopping trips, house chores, yard work, or pet care. Remember that friends and neighbors want to help and often do not know what would be of assistance. This is a time to put pride aside and be grateful for the assistance of others. There is no doubt that you have helped others out in a crisis and now let them return the favor by accepting assistance.
What would your self-care wish list include; a few minutes of music, reading, walking, resting, having a massage, or haircut? Consider what will help you “recharge” for your next session of caregiving. Then determine what you need to do so that you can have your “recharge” time. It may mean having someone sit with your loved one to keep them company so that you can take care of yourself.
Preplan, Avoid FUDGE
Preplanning is a strategy to have backup plans and options available when an unanticipated turn of events surfaces. This would include having a list of backup caregivers/home care agencies, a “stash” of supplies/medications, extra food, or other items that could disrupt the caregiving routine. Don’t forget backup drivers and other roles that you depend on. Strong preplanning will help minimize a crisis.
Explore caregiver and senior resources in your community; check out faith-based organizations and diagnosis-specific associations (Alzheimer’s, American Heart Association, Cancer-related organizations…). Remember to discuss specific concerns with your healthcare provider for additional referrals, resources, and support. Minimize your suffering from FUDGE by preplanning.
Support a caregiver
Determine what you can do to ease the role of caregiving. It can be as simple as sending cards weekly, calling, and letting the caregiver know that someone thinks of them. The most helpful and meaningful things caregivers wish for are; meals, grocery deliveries, and attending to chores where someone volunteers and does not wait to be asked. Not everyone feels comfortable being around the loved one when they are ill or declining, yet caregivers need support. Consider stating to a caregiver “I am going to the supermarket, give me your list”, I will mow your lawn today/take out and pick up your trash cans”, and “I will fix your porch light today.” Leave a surprise you know the caregiver or loved one would appreciate. Be creative in lessening the burden and helping a caregiver smile. Remember that caregivers are suffering from FUDGE and need your assistance.
Caregiving is a work of the heart!

Resources
Military Veteran Caregiver Network

Spring Cleaning and fall prevention; who knew they went together? A third of community‐dwelling people aged over 65 years fall each year. Falls can have serious consequences including restricting activity or institutionalization[1]. Most seniors report that falling is one of their major concerns. Fall prevention should be on everyone’s radar, and spring cleaning is a great way to personalize the fall prevention initiative.
Fall-related injuries impact one’s quality of life, often resulting in loss of independence, decreased mobility, and, in some cases, early admission to a nursing home. The fear of falling can cause people to limit their activities, leading to reduced mobility and increased risk of falling[2]
What is a fall?
There are several definitions for falls, yet in reality, it is where an individual comes to rest inadvertently on the ground. Falls may result from a risk factor that can be anticipated such as altered mental status, an abnormal walking pattern, a balance issue, frequent toileting needs, or high-risk medications. There are also unanticipated risk factors that can result in a fall such as a seizure, stroke, or fainting episode. Environmental factors such as uneven pavement, water on a walkway, electrical cords, tripping over a pet, and poor lighting are other leading causes of falls.
Who is at risk?
Individuals with dementia, impaired vision, a history of falls, and depression, and those living with a spouse are at a higher risk for falls. Physical and environmental factors impact the rate of falls. Studies reveal that individuals who have fallen once will likely fall again. Working collaboratively with your healthcare professional will help in determining your risk of falling and actions to take to reduce your risks.

Spring Cleaning
Spring cleaning is a critical way to address the environmental factors at home. Minimizing these environmental hazards is a great way to increase the individual’s level of confidence as it relates to falls. For spring cleaning to be effective and successful, there needs to be active participation and engagement of the resident and/or caregiver. The process to identify and remove environmental hazards will take time. This is dependent on the size, condition, and amount of clutter in the residence. It’s best to start in those areas that present the most risk, kitchen, halls, bathrooms, and bedrooms.

What to look for?
Start at the bottom by looking at the floor; is it in good condition (uneven flooring,? Are there trip hazards (electrical cords, furniture barriers, and inability to safely utilize a walker, wheelchair, or rollator?
Remember that falling is not a normal part of aging! Many falls can be prevented. Spring cleaning is a great way to minimize fall and trip hazards. Make your spring cleaning meaningful by focusing on keeping your home free of fall hazards. Reduce the chance of a fall.

Action Steps
- Consider obtaining a fall predictive device/alarm, especially one that alerts someone else of your fall
- Repair or install flooring for easier mobility
- Remove scatter rugs and runners
- Consider the individual’s dominant side with equipment and furniture placement
- Remove unstable furniture
- Consider the installation of grab bars
- Determine if frequently used items are within reach – rearrange to keep items within reach
- Review footwear – Nonslip, comfortable, well-fitting footwear
- Discuss with your medical provider:
- Need for physical and occupational therapy to preserve physical function, assess balance, and perform a detailed home fall prevention assessment
- Medications that may have an associated falls risk (those that cause drowsiness, dizziness, or confusion). Advise if you get dizzy or lightheaded when you go from a sitting to a standing position
- Need for vision screening
- Need for assistive devices
- Ensure adequate lighting and night lights are available. Assess during the evenings to address shadows
- Check for loose or uneven stairs and the condition of handrails
- Eliminate clutter; discard unused and broken items, keep the floor and counters free of unneeded items
- Keep wheelchair wheels in the “locked” position when stationary
- Keep floor surfaces clean and dry
- Lower the mattress to the floor, especially helpful for shorter individuals
Yes, spring cleaning and fall prevention are very closely tied together.
Resources
Check for Safety – A Home Fall Prevention Checklist for Older Adults CDC’s tool to assess your residence
Older men at higher risk for falls-related skull fractures: study
Addressing at-home hazards may cut falls risk by a quarter, Cochrane Review findsStudy: Falls rate nearly 50% for U.S. seniors with dementia; 3 factors raise risk
[1] Environmental interventions for preventing falls in older people living in the community
[2] Programs and Policies to Prevent Falls in North Carolina

The guest post was written by Ed Carter.
How do you help a senior loved one when you live far away? There is no one easy or right answer for everyone. There are some tactics to consider when you feel your loved one needs your continuous presence for care and attention. Moving closer to your senior loved one is not an easy decision or one that should be taken lightly. Despite the fact that some caregiving coordination can be done from afar, along with the creation of emergency plans, it’s often easier for caregivers to move closer to their loved ones to provide help on a regular basis.
Moving closer to your senior loved one requires careful preparation. You’ll need to figure out what kind of changes will be necessary once you arrive for yourself and your loved one. Consider if additional services such as home health are required. Determine if they can remain in their residence or if they’ll need to sell their home. Caregivers need to take care of themselves in addition to their loved ones. Explore services such as meal preparation, cleaning services, or other supports that will lighten your burden. Here are some tips to help you with your planning.
Do Your Homework
Buying a home in a new area requires homework, and it will also help to give you peace of mind about a smooth process. Map out a step-by-step plan that includes an assessment of your financial wellness. Download a credit monitoring app to help you keep track of your score (and possibly boost it). Look into getting pre-approved for a loan. This makes the home buying process quicker and will reduce some anxiety about the cost. To get a better idea of the homes in your price range, tour virtually or in person. Lastly, check out this helpful guide that tells you everything you need to know about mortgages.
Keep Your Loved One’s Home in Mind
Of course, if your loved one owns their home, you’ll need to take that space into consideration too. Decide if the residence is too much for you or your loved one to maintain; or if there is a need to save money by moving to an apartment or senior community. You’ll need help listing the property for sale. Whether your loved one stays or moves, you’ll also need to hire some services to make adaptive changes, clean, or make repairs.
The roof and gutters are a significant consideration, since they’re a big factor for homebuyers and can affect the foundation. Cleaning the gutters twice a year is crucial to keep leaves and other debris from creating blockages and creating leaks. Since this can be a dangerous chore, hire a pro to do it safely by searching online. The cost typically ranges from a few hundred dollars to $350 depending on the size of the job and location.

Set Up Some Resources
Moving to a new home and tackling your loved one’s needs means there will be a lot on your plate. It’s a good idea to set up some helpful resources before you even arrive. Get to know their neighbors, and search for senior services online (extensive list of resources) that will be useful to your loved one, such as free rides, grocery delivery, and cleaning services. Look for useful apps that keep track of medication times or stay in touch with their family and friends. The more tools you have ready to go, the easier it will be for you to hit the ground running when you get to your new home.
Helping a senior loved one can take a toll on your mental and physical health. Make it a priority to take care of yourself as well; physically and spiritually. This will it allow you to stay focused as a caregiver and will help you keep your loved one safe. Remember that you can not be an effective caregiver if you are not at your best. The airlines remind you to put on your oxygen mask in the event of an emergency before helping someone else.
Ed Carter has worked with clients of all ages, backgrounds, and incomes. About 10 years into his career, he saw a need for financial planners who specialize in helping individuals and families living with disabilities. edcarter@ablefutures.org
Judith Sands has over 30 years of experience as a healthcare professional and is a recognized authority in the areas of quality, risk management, and patient safety. Her current focus is on ensuring patient safety, care coordination, and bringing dignity to end-of-life care. Don’t hesitate to reach out!
Feature image from Pexels

Modesty in healthcare seems like an oxymoron. There are so many cartoons and comics poking fun at someone’s uncovered backside, and just about everyone can share an experience about being “exposed” in a healthcare setting. Modesty in healthcare: privacy is urgently needed. The lack of modesty protection in healthcare is a troubling issue, especially for those who have suffered from sexual assaults, physical disfigurement/deformity, those with strong religious or cultural beliefs relating to modesty, children and teens, individuals transitioning, and those with poor body image and are prone to embarrassment. Unfortunately, modesty and privacy in healthcare are in short supply and are known barriers keeping patients from seeking care and treatment.
Modesty is learned through culture, religion, and community standards. It is often associated with discouraging sexual attraction, a sign of respect, and modesty standards vary widely. Too often in healthcare, modesty has not been a key issue for healthcare professionals, and in some cases that fosters the relationship divide between the healthcare professional and patient. Clinical convenience has outweighed the patient’s expectations for dignity, modesty, and privacy.
Lack of modesty in healthcare is anxiety-provoking
Seeking medical care or diagnostic testing are anxiety-producing events. That anxiety is magnified for individuals with modesty and body image issues. The sentiment expressed by some patients is that the thought of being exposed (even under anesthesia), is a loss of self-control. The fear of potentially having their privacy violated can contribute to a delay in seeking care and treatment. These anxiety issues are not skewed by sex, age, or religion.
Modesty: Keeping it private
Modesty in healthcare impacts every patient! It goes beyond keeping breasts and genitals covered; it includes the respect and dignity offered when addressing, examining, or treating a body part. Cultural sensitivity, having the awareness associated with how various cultures view protecting modesty and being sensitive to the individual’s specific concerns is crucial in building and maintaining trust between patient and the healthcare professional. When in doubt, ask what would make the patient feel more comfortable.
It is a two-way street and patients and their caregivers should feel empowered to speak up and share concerns. It may not be easy to do, yet it reminds healthcare providers and staff that patients are human; they expect dignity in treatment and caregiving. Healthcare professionals must provide for modesty, and be sensitive to privacy issues, especially when caring for minors or a member of the opposite sex.
Common courtesy
Unfortunately, healthcare providers and staff are often rushed, focusing on the tasks at hand, and in the process fail to address key patient concerns. Patients and family members with concerns may find it difficult to share, yet the provider will not know your preferences if you do not express them. Healthcare professionals have seen many “private parts” and over time have become desensitized to a particular patient’s anatomy. By no means does this excuse healthcare professionals from being respectful or sensitive to a patient’s need for privacy and modesty.

Privacy needed in healthcare – modesty garments an answer
Modesty garments are not yet the standard of care. The movement of individuals learning about modesty garments is growing. Patients are openly expressing their discomfort and anxiety about being “exposed” while receiving care. In return healthcare facilities and providers are being forced to “see” and address modesty from the patient’s perspective. Patients will seek out organizations and providers that acknowledge and address the patient’s anxiety and respond to the customer’s requests to address the issue of modesty.
COVR Medical established by an orthopedic surgeon is committed to protecting and ensuring patient privacy, modesty, and comfort before, during, and after a surgical or medical procedure. The company has several medical-grade garments available that fully cover the genital area.

What you should expect
- Knocking on exam room doors and asking permission before entering
- Curtains in exam rooms to block the view from hallways and provide a greater sense of privacy
- Having a chaperone of the same sex when intimate body parts are examined
- Drapes or gowns that fasten to help patients feel less exposed, including a second gown or drape
- Offered modesty garments for procedures that may expose the groin/genitals
- Being asked for your consent before being touched told what will be done to you before actually performing the exam or treatment
- Speak up & ask!
- Does underwear have to be removed?
- Will a shave or prep be performed and who will perform it?
- Will my private parts be exposed and who will see them?
- What will you do to maintain my modesty?
- Ask for a modesty garment if it was not offered
- Ask for a same-sex staff member to assist with toileting or dressing
- Express any concerns upfront
Resources
The naked patient: Modesty movement won’t take it lying down

April 16th is designated as National Healthcare Decisions Day: make your wishes known! It’s the time to educate the general public and healthcare professionals about planning and preparing for future healthcare decisions; making wishes known. Too often individuals do not want to think about their mortality and fail to outline their advance care wishes; this applies to everyone, not just retirees. On the flip side, there are family members wrestling with how to address the topic with aging loved ones. National Healthcare Decisions Day was established to address the proverbial “elephant in the room,” associated with discussing the critically important process of individuals making their healthcare wishes known. The next step is to outline their Advance Directive care choices, for others to follow should they be unable to articulate their wishes.
National Healthcare Decisions Day – Finding the right time
During the upcoming holidays, while families and loved ones gather again in person it’s an ideal time to discuss healthcare wishes. In many cases, this will be the first time that the in-person gathering may be taking place in two years. It will be more evident that the impacts of chronic illnesses, COVID-19, and decreased social interactions have taken on individuals. This is a great time to bring up the issue of Advance Directives. The conversation opener can be mentioning that National Healthcare Decisions Day is April 16th and ask about who has made their wishes known.

Making your wishes known, speak with the provider
Centers for Medicare and Medicaid Services (CMS) guidelines reimburse physicians or other qualified healthcare professionals for having the face-to-face discussion about the patient’s health care wishes if they become unable to make decisions about their care. This may be an alternative starting point for some by including the healthcare provider in the discussion and getting a clearer clinical picture of the loved one and issues that are particular to that individual.

Resources
There are a number of resources to facilitate and help in defining your Advance Directive wishes. Many of these resources are also available in a number of foreign languages.
Advance Directives, health care decisions expressed and documented by an individual, officially serve as the instruction for future events. These documents remove the onus of decision-making from the family and loved ones at the time of a medical crisis. Loved ones should not be left guessing what you might have wanted to be done in a medical crisis. Help your loved ones fulfill your wishes by providing instructions through the completed Advanced Directive.
Taking action
Advance Directives should be updated; it is a good practice to review your wishes annually or after a major change in health status. The revised documents must be shared with the Healthcare Champion (Surrogate), and your physician (medical team). Upload them to a registry if available in your state. Avoid placing Advance Directives in a safe deposit box since they will not be accessible in an emergency if the bank is closed. Consider uploading to your smartphone for backup.
#NationalHealthCareDecisionsDay
#HealthCareDecisionsDay

Regret, according to Merriam-Webster is sadness or disappointment caused especially by something beyond a person’s control or, an expression of sorrow or disappointment. Often individuals self-blame, dwell on the sadness and disappointment associated with prior decisions, and have missed out on events, and experiences. Too often individuals focus on things beyond their control. Avoiding regrets: there’s no turning back the clock, requires recognition of one’s focus, and making a conscious decision to redirect one’s energies from the past to the future. Avoiding regrets is an individual choice.
Avoiding Regrets: There’s No Turning Back the Clock
There are no “do-overs” in life. Despite our wishes to “turn back the clock” and make different decisions or actions given our 20:20 hindsight, we have to acknowledge the regrets and learn to live with what has transpired in our lives. Don’t spend anymore valuable time on “would,” should” or “could”, it’s over, and despite how much we want a different outcome from the past it will not happen. The “clock” has ticked forward. Recognizing our feelings associated with regrets is a reflection of the past and not the future.
Time to Adapt, You Can’t Turn Back the Clock
If you have been consumed by regret, sadness, anger, shame, anxiety, and disappointment with past deeds or how you perceive life has “treated you,” there is still the option of reframing your experiences and developing a different outlook. It’s time to put closure on the past, no matter how painful it is. Avoiding regrets is a personal choice. Reflect on all the time you have spent focused on regrets, and acknowledge that the time has been spent and now you are actively going to refocus on the future. It may be scary and somewhat anxiety-provoking.
Priorities change over time, and this is the time to focus on the here and now. When time and energy are spent on something productive where you can see results, you will build on this positive energy and feel better. Your regrets are lessons that you learned along life’s journey.
Avoiding Regret Action Steps
- Realistically acknowledge your role in a disagreement that resulted in a fractured relationship. Apologize for what you have done and do not excuse yourself.
- Do something to “bury” your regrets towards those that you cannot apologize in person. Formalize the process by writing your regrets and then burying or burning the list
- Commit to new, positive ways of thinking, focus on the positive that you have accomplished
- Donate to a charity or volunteer, expend you energy in meaningful ways
Remember, it is not always about you and others are also suffering, especially these days.
Resources
21 Ways To Stop Regretting The Past And Finally Move On
Regret can seriously damage your mental health – here’s how to leave it behind
How to avoid regret: What a doctor wishes people knew about living, dying well

Individuals and families often ask me, “How to live while declining?” Loved ones know, even if they don’t discuss it with friends and family members, that they can no longer do all the things they could do earlier in their lives. Recognizing that their body is “betraying” them is jarring; the inability to perform all the things that they were physically capable of doing a few months ago, last year, or a few years ago can be disconcerting. How to live while declining? Despite the physical challenges that individuals encounter, it does not mean that they want or need to give up on living. These individuals still have a lot of living while their physical status changes.
How to live while declining?
To continue living meaningfully, despite the physical changes, requires creativity and a change in perspective. It is not about “what I cannot do,” rather, it is about “what I can still do.” You can still live well while your physical health declines. Individuals and families need to change their perspectives, focusing on making the best of the time that is still available.
Preplan & Do!
Sometimes we are surprised by our body’s physical decline, especially if it has a sudden onset or is a result of some type of trauma. For others, the physical decline may be the natural progression of aging or a medical condition. Have you ever considered or thought about what you would do as you age? Do you have a bucket list or wish list of things you want to accomplish? This is the time to review or develop that list. Unfortunately, there may be items that you will not be able to accomplish. Live while declining and focus on what you can do!

Stay Engaged
This may be the time to write, arrange photo albums, go through paperwork, and get your affairs in order. This can also be the time for engaging in hobbies or spending time learning something new. Many organizations routinely present various types of content and often have recorded programs available on demand.
Many wonderfully positive things came about from the pandemic, the proliferation of virtual educational, religious, and recreational programs, many of which are free.
- You may not be able to physically travel, yet there are a host of programs focusing on national and international city tours, historical sites, houses of worship, and parks and landmarks.
- There are programs dedicated to book reviews, entertainment, movies, opera, history, current events, language, health, business, and music. Many social, religious, professional, advocacy, and non-profits also provide content.
- YouTube isn’t just for kids. There is extensive content for just about any topic you can imagine, from how to perform a home repair, cook, clean, garden, find a bargain, score a deal, entertain, amuse, and, even surprise you. Once you start searching, you may never stop.
- For those looking for more formal content there are many massive open online course (MOOC) educational content providers including Coursera, Udemy, Future Learn, content is often free and available in many different languages form institutions around the world.

Actions & Practical Time Tested Tips
- Advance Directive – be sure that your wishes and preferences are documented and those that you have named as surrogates are aware of your Advance Directive and will honor it. Consider if any updating is needed
- Support – counseling, in-person or virtual support groups. Realize, you are not the only one who is experiencing a physical decline, and you do not have to go through this alone. Family members and caregivers, this applies to you as well. Your roles may be changing, and you need to be supported on this journey as well
- Request physical therapy and occupation therapy consults, it is very important to preserve physical function and build where possible. These professionals are wonderful at suggesting adaptive devices and helping to make you home environment safer
- Focus on what you can do! Do what you can physically, stay as active as possible. Preserve range of motion
- Put some seeds in a pot and watch them grow, marvel at what you and Mother Nature can do together
- Do something for someone else; it can be as simple as having a coffee chat, calling, sending a card, or doing something to lighten their load. You are still able to connect with others; you will get more out of the experience than you think. It’s not always about you!
- Engage your mind is something that will bring a smile to your face and joy to your soul!
- Check out Caregivers and “Lucky Life” a gentle reminder that life is made up of so many different experiences.



I was fresh out of college, and new R.N. working the night shift at the hospital. I don’t think anyone finds love when they go looking for it. It just comes out of nowhere, usually from someone or someplace you least expect it. And so, this is what happened to me. One of the nurses I was working with fixed me up with this guy she knew. A love story in the making.
A love story in the making
During our dating, he treated me like a princess, took me to the submarine races at Ft. Lauderdale beach, and brought my father Carvel ice cream cakes every other week. Much to my surprise, I already knew Louis’ mother and sister; I just didn’t put the pieces together until he surprised me on a dinner date with “you’re meeting my parents in 15-minutes.” All of the evidence pointed to Louis being a good catch. However, in every relationship, there is always that one little thing that seems like nothing so you ignore it. You dismiss it because you love him. Deep down, you know that you can change him; you’re the most important person in his life and naturally, he will come around to see things your way. And we all know how willingly a husband changes for his wife. A love story in the making.
A big wuss!
The love story continues. Despite Louis’ many wonderful qualities, the most prominent one is that he is a wuss when it comes to needles. I’m not talking about the ordinary “I don’t want the shot, but I’ll get it because it’s good for me” wuss. I’m talking about being President of the Big Wuss Club, needle-phobic, full-on wuss. My first clue was when we went to get a blood test for our marriage license. At Louis’ insistence, he put his arm in some convoluted twisted armbar and then had me sit on his arm to prevent him from moving/escaping. I remember the blood draw took almost 90-minutes, and I’m pretty sure he laid on the gurney for at least 45-minutes to “recover from the trauma.” Instead of doing the logic in my head and running for the hills, I went on to marry this Big Wuss.
Loving a big wuss
As a loving and caring wife, I like to think of myself as understanding and compassionate. As a nurse, I understand that an injection, especially with a 26 or 28-gauge needle (a very small diameter needle), is less traumatic than getting bitten by a mosquito. What I didn’t fully appreciate is that Louis’ fear is a phobia. By definition, a phobia is an unfounded fear of something. It’s not rational and can’t be explained logically, but in the mind of that person it’s very real and all the logic and explaining doesn’t change anything. After 36 years of marriage, I have stories of Louis and shots (or lack of) that can fill a book. Early on in our marriage, we were walking in the mall and I noticed Louis stopped to watch a girl get her ears pierced. Bad move Lou! Everyone except Louis knew what would happen. Within seconds of hearing the click of the piercing gun, Louis found the floor. Yep, he fainted in public. You see, part of his phobic response doesn’t have to personally involve him. Louis didn’t get his tetanus booster for 35 years and when he finally did, he insisted that it be done while he was asleep during a colonoscopy. Oh yes, you read the tea leaves correctly. He needed an IV for the colonoscopy and that too in another needle-phobic story!
A vaccine of love on the horizon
It’s March 2020 and the COVID-19 pandemic is in full force. We don’t know much about it and everyone hopes to quickly put it behind us. In this turbulent time of uncertainty, the one thing I’m willing to bet on is that the solution will involve a vaccine given by a jab in the arm. My mind is conflicted; on one hand, we’ll finally be able to socialize and get back to a more normal lifestyle but to do this will require Louis to get a jab, or two, in the arm. Will he voluntarily take the shot or will have I have to put him in a straitjacket? Louis is intelligent; he understood that all of the data indicated that getting the vaccine was the solution. He talked to me for months, ad nauseam, about getting the vaccine. He could have written a master’s thesis from all of our discussions. Regardless, I understood that this is how he was mentally preparing for the inevitable. If this is what it took to get him vaccinated then I would play along. The love story continues.

Getting vaccinated
It was a good sign when Louis said he wanted the vaccine. Since we’ve been married, the process has always been Lou moving around for 20-45 minutes while I tried to calm him down long enough for the nurse to jab him. Yes, I know it sounds silly but keeping in mind he has a phobia. Marriage is about trust and respect. He trusts that I know how to handle his phobia and that I will respect his “guidelines” when he’s getting a shot. Unfortunately for Louis, I am also a nurse and everyone knows that nurses have lots of things to do and we work on our terms; there’s no time to dilly dally! Sit down (because it’s closer to the floor for when you faint), roll up the sleeve, bam! Next! Louis did get his two jabs of the Moderna vaccine. He didn’t faint or fuss. However, watching his face go pale after receiving the injections …. priceless. That’s the man I married.
Get the vaccine! Figure out what works for you or your loved one, reconcile your fears, and just do it.
Remember, It is not recommended you take over-the-counter medicine – such as ibuprofen, aspirin, or acetaminophen – before vaccination for the purpose of trying to prevent vaccine-related side effects, per the CDC.

Resources

Throughout this pandemic, I have been frustrated by the politicization of the public health issues associated with masking. I have cried out when seeing masks used as chin warmers or shuddering when people take off their masks to talk to others. Don’t they get it? My ideal imaginary mask monitoring job may soon be gone! Oh, what a hopeful thought.
My job: mask monitor
My nursing and infection control trainings are front and center each time I watch TV, go to the store, or out in public. What’s so hard about mask-wearing? Cover your nose and mouth to minimize spreading droplets. Protect yourself and others. My desire to contain the spread and help us return to some “normalcy” is overwhelming. Considering the valued guidance of my hero Dr. Fauci, and the CDC, nothing should be simpler. My ideal imaginary mask monitoring job has sustained me through the pandemic.
My friends and family eagerly wait to hear about my encounters with a mask-wearing “flunky.” My report, a bit of dark humor, includes the name and type of the establishment that is relaxed in enforcing or addressing the mask mandate, the description of “mask offender” and the associated observed “infraction” (an exposed nose or a mask used as a chin warmer?) Occasionally, I will admit that I mentioned to some offenders that their mask appeared to have slipped, to others, I readjusted my mask while facing them in hopes that they would get the message, and sadly on other occasions, I expressed my frustrations to my husband. His response: “the only way you will fix that situation is with the application of duct tape.”
Masks on TV
Watching medical shows and sports coaches on TV has been another source feeding my secret mask monitoring role. Scenes of the “ER” where staff are treating patients during the pandemic without a mask, or the sports coach taking off the mask to speak to players, watching some players on the sidelines with masks while others are barefaced, sends my blood pressure soaring and those around me are preparing for my rant.
Toilet training is easier than mask training
For those who have had the joy of toilet training a toddler, there are several approaches. You work with the toddler on modeling the desired behavior or resorting to bribing and rewarding for the appropriate toileting behavior. Yes, I was reminded that no child went to college wearing diapers, that finally, the child figures it out, typically in a few months. Dog trainers also note that it takes under a year to turn the cute little puppy into an adorable command responding dog. So, what’s so hard about learning to correctly wear a mask in public that covers both the nose and mouth? If you were able to get a driver’s license or have the intelligence to vote, what is the difficulty with learning to correctly wear a mask?
My ideal imaginary mask monitoring job may soon be gone!
I am overjoyed that vaccines are now more readily available and that I served as a volunteer vaccinator. More people are getting vaccinated and herd immunity is within reach. I am losing my ideal dream job to an app! Software companies already have AI to detect non-masked individuals (LeewayHertz, AVIGILON). Help make my job obsolete! Keep those masks on for just a bit longer! Remind others to do the same. Collectively, we can make a difference. Take care of each other and let’s not give up while we are approaching the home stretch.
Action steps
- Wear your mask!
- Get vaccinated and help someone else with making an appointment or getting to the vaccination site
- Consciously express gratitude when getting vaccinated
- Make a donation to a foodbank or other charity in honor of getting vaccinated
Resources

Serving as a volunteer COVID-19 vaccinator with the CapRAC Healthcare Preparedness Coalition (NC) has been one of my most rewarding professional experiences. One would think that these roles are plentiful, in reality finding the public health entity seeking volunteers is challenging and not easy to find. In North Carolina, finding the volunteer COVID-19 vaccinator position involved some detective work, and stamina to complete the application and training process. The reward of being approved as a volunteer COVID-19 vaccinator and signing up for my first outdoor, drive-by mass vaccination shift was exciting.

My first volunteer COVID-19 vaccinator assignment
The weather was dismal, 340, rainy, and windy! My co-vaccinators and recorders were amazing. They included nurses from a variety of settings, physicians, and county employees all dedicated to the mission. We had a tent that covered the supplies and kept our documenters dry. As I approached each car:
- I ensured that the car was in “park”
- Reviewed the key clinical issues
- Gave the appropriate documentation to my documented
- Obtained the prefilled syringe of vaccine and adhesive bandage
- Administered the shot
- Disposed of the supplies
- Sanitized
- Imparted the precious white CDC vaccination card
- Provided follow-up instructions
- Got ready to repeat the process with the next carload full of hopeful individuals.

Greeted with gratitude
Expressions of gratitude began when the windows were rolled down, and individuals presented their arms even before I had the opportunity to say anything. “Thank you for being here in this weather,” “you are angels to be doing this,” “you have no idea what this means to us.” Such comments were heard from each of the individuals in the vehicles. Some individuals even wanted pictures marking the event’s significance. No complaints relating to wait times or registration frustrations were shared, just expressions of gratitude, so grateful for obtaining the vaccine.
Covid-19 vaccination lighter moments
Despite the fast-paced vaccination process, some situations made me smile. Throughout the pandemic, my deep-down secret desire was to be the mask monitor. Now was my “mask monitoring” wish was coming true. Despite signage and advance notices, it was surprising the number of individuals who drove up without wearing their mask or wearing it incorrectly. No chin warmers in my line! No mask, no shot! Pointing to my mask and waving the syringe quickly got the mask in place and the vaccination process rolling.
Given the cold weather, several male vaccination seekers wore leather biker jackets. In their eagerness to get vaccinated, they were surprised that they needed to remove the jacket. On more than one occasion, I had to remind them that the needle on the syringe could not go through the leather jacket! Several individuals asked if it mattered which arm they got their shot in. Others asked if they should get the second shot in the other arm!
COVID-19 vaccination touching moments
Several of the cars rolled up with the driver having a loved one in the passenger seat suffering from dementia. It was obvious that it was a big effort to get this individual to the vaccination event. The expressions of relief by the caregivers at the end of the vaccination process were very touching. There was a van load of individuals from a group home, each came out of the van, sat in a folding chair for the vaccination, and returned to the van. Teammates came to assist so that the process could be expedited. Teamwork and collaboration were evident throughout the day.
Did you give me the shot?
Given the small size of the needle used in the vaccination process, many individuals shared that they did not feel the shot, and did not realize that it was complete. Often stating “this was nothing compared to what I was expecting.” Once again, comments of gratitude and hope followed. Urging them to share this experience with their friends who may be reluctant to get vaccinated.
A family and friends volunteer experience
During orientation, I learned that non-clinical individuals were being recruited to help with traffic flow and documentation at these mass vaccination events. I became a recruiter, engaging my husband and close friends in helping make a difference in our community.
During one of our “couples” events, I “injected” some humor into the process. My husband was involved with traffic flow. He was the next individual that my carload of vaccinated individuals would encounter. To set the stage, my husband is needle-phobic; he won’t even look at the TV when an injection is given.
For a few of those that mentioned that they did not feel the shot, or were especially complimentary, I asked them to share their experience with the “traffic guy” ahead. Explaining that he is terrified of shots, and never had the opportunity to hear directly from any of my “patients.” These individuals roared with the prospect of having some fun at his expense. On the ride home, my husband shared his experiences of the day, including the fact that he had several individuals who shared with him that the process was painless and the nurse giving the shot was great. I confessed that he was set up. Everyone involved in the ruse had a good laugh.
I will miss this role
Vaccines are now being distributed in greater numbers; pharmacies, clinics, and other locations are augmenting what is being done at the mass vaccination sites. The National Guard is taking a greater role in the process, and I am being demobilized from my medical reserve role. Serving as a vaccinator has been so meaningful, my actionable way to strike back at COVID-19, give hope to others, helping to open back the community.
Action steps:
- Signup to get vaccinated
- Help others with the registration process. There is a movement of individuals committed to helping others with the process. It is important to note that who is eligible for the vaccine differs by state and in some cases also by locale. In most cases, appointments are needed, yet the first-come-first serve events are surfacing. At the end of the day, some locations will open up the vaccination effort if a few extra doses are available. Many states have their own locator along with pharmacy chains, Vaccines.gov, Plan your vaccine, Find local COVID vaccine locations
- In honor of being vaccinated make your contribution! Consider making a donation to a food bank, drive someone for a shot, take some action to promote wellbeing in your community
- Wear your mask! Wash your hands and keep the physical distance from others
- Guard your white CDC-vaccination record. Do not post the picture of your vaccination record online, it contains personal identifying information. No doubt that this will be a “passport” of sorts, proving your vaccination status

Vaccine envy is morphing into immunization guilt, a new phenomenon. For those who are meeting the vaccination eligibility criteria, and are lucky enough to score one, they are transitioning from being vaccine envious to now expressing immunization guilt. Despite being very grateful for the opportunity to get vaccinated, they are very conscious that there are others in need. These include individuals with medical conditions that do not meet current eligibility criteria. Younger individuals performing home caregiving for family members are also experiencing vaccine envy.
Individuals with immunization guilt are very sensitive to those challenged by the registration process, shortage of vaccine, and having difficulty getting to a vaccination site. Immunization guilt, similar to survivor guilt, is a new phenomenon gaining traction among those who have obtained the vaccine.
Vaccine bragging rights are making headlines by individuals who have “beat the system” in obtaining their vaccine. These types of social media posts reflect the extreme opposite of immunization guilt. The disregard for equitable vaccine distribution has resulted in overwhelming negative publicity for these “line-jumpers,” and the vaccine administrators.
Nurses expressing immunization guilt
Nurses are one of the key front line professionals caring for those suffering from COVID-19. In their role, they are providing the most ongoing direct patient contact. It is a “no-brainer” that these professionals should be afforded the best available protection while caring for COVID-19 patients. Yet, there is a segment of the nursing professionals expressing that they do not feel deserving of the vaccine. Expressing that there are others who should come before them. Nurses are altruistic by nature, often placing patient’s needs before their own. Experiencing immunization guilt should not be a suffered emotion.

Nurses as role models
There is a larger group of role model nurses who are getting immunized. Thereby, demonstrating vaccine safety, and the importance of protecting themselves and others. There have been a significant number of nurses, first responders, and other healthcare professionals that have succumbed to COVID-19. This strains the healthcare delivery system for everyone. The lack of available professional staffing means that EMS and facilities will be challenged in providing needed direct patient. Nurses are taking a positive stand, setting the example that others should get in line to be vaccinated.
Help with herd immunity, counter immunization guilt
For those suffering from immunization guilt, you are part of a growing group that is helping the country on the journey to meet herd immunity. You are the example others need to follow to help the country reach the still elusive magic number. Herd immunity will be reached when over 70% of the population is immunized.
Action steps
- Continue to wear your mask, maintain the physical distancing and wash your hands frequently
- Help someone else get a vaccine by assisting with the registration process or transportation
- Say a prayer of gratitude for having received the vaccine and pray that others will be able to get theirs’ soon
- Consider a food bank donation or other contribution in honor of being vaccinated
- Protect your immunization card, don’t take pictures of it and put it on social media. It contains key pieces of your identity and makes you a target for identity theft

Resources
Guilt is the biggest side effect of receiving the COVID-19 vaccine

There is a new social trend surfacing, vaccine envy. This emerging movement is surprisingly pitting loved ones, friends, neighbors, and acquaintances against each other. Vaccine envy: “where’s mine?”, is one of the hottest topics of conversation. Typically it includes the challenges individuals experience in trying to locate and register for vaccine administration, the associated vaccine administration wait times, and the fear that there may not be sufficient vaccine at the time of your appointment
Vaccine envy, is being expressed by caregivers of those loved ones being cared for at home, and individuals with chorionic health issues that do not quite fit the established criteria. Some are expressing resentfulness over the criteria. Why is priority given to prisoners, tourists, foreigners, and those who found a way to game the system? Therefore, pushing them further to the back of the line. Where’s mine?
Envy
Envy, as defined by Merriam-Webster, is “painful or resentful awareness of an advantage enjoyed by another joined with a desire to possess the same advantage,” a discontented longing for someone else’s advantages. That clearly describes the sentiments of vaccine envy: where’s mine? Do you have pent up negative feelings; do you begrudge others in your frustration, disappointment, and longing for the vaccine? Is someone you know expressing such sentiments?
Aristotle defined envy as pain at the sight of another’s good fortune, which also clearly illustrates vaccine envy; others have what we ought to have. Envy was one of the most potent causes of unhappiness according to Bertrand Russell. Envious individuals become unhappy and bitter by these feelings, taking out their frustrations on others, often with harsh words.
What is vaccine envy?
Today, that advantage is the earlier access to one of the COVID-19 vaccines. Do you begrudge your state’s established distribution plan that may place individuals whom you do not think should be vaccinated before you? Realizing that some states (Florida, New York, North Carolina …) are giving the vaccine to non-state residents, tourists, and non-US residents before you; placing you further back in the line. It can be very disappointing and cause some envy. Consider your first reaction once you hear that a friend has “scored” a vaccine registration appointment; congratulating them on their good fortune or are you thinking of your misfortune, that it is not your time?
Taking Action: Trying to get vaccinated
Check your perceptions and perspective. Consider how are you coping, what emotions are you experiencing? How would others view your words and actions?
Once you meet the vaccine administration eligibility criteria, the process of actually getting registered can be very frustrating.
- Sign up for alerts from the media relating to vaccines
- Share alerts between friends
- Call the free 211 (information and referral service) and 311 (non-emergency town services)
- Enter Vaccine + country into your internet search bar for updated county resources
- Check your County & State health department websites for updated information
- Consider going to a neighboring county
- Check with clinics and health systems (some health systems have set up waiting lists. Check your patient portals)

Now that I have been vaccinated
This is not the time to let your guard down, remember that immunity is not instantaneous. It takes several weeks for your body to build antibodies, and you are still susceptible during the this time period. In fact, two vaccine doses are needed for optimal protection.
- Continue to wear your mask and practice physical distancing
- Show gratitude, express your good fortune positively
- Say a prayer of thanksgiving/gratitude after getting your vaccine
- Helping others register or get to their appointment
- Donate towards administration fees that may not be covered
Resources
When can I get my COVID-19 vaccine? See a state-by-state guide
State COVID-19 Vaccine Prioritization and Phase of Vaccine Distribution, as of January 11, 2021
As we usher in 2021, our wish is for a brighter year. Hope is a four-letter word. It is the spirit that will guide and sustain us as we begin making plans and thinking ahead. Hope, according to the Oxford Dictionary, encompasses expectations for the future along with feelings of trust. Hope is the four-letter word we need now more than ever. There are many four-letter words we are admonished to use, hope is the four-letter word critical to mental well being

A Four-Letter Word: Hope is…
Hope is the four-letter word that keeps us getting up in the morning, caring for ourselves and others. Hope is the optimism needed to make it through challenges, conflicts, loss, and hard times; despite hardship, we anticipate a brighter outcome. Resilient individuals, tend to hope more. They anticipate current challenges becoming lighter, and looking forward to the return of “brightness.”
Hope is individual; each of us has our own wishes and dreams. Some of these may be more realistic than others, yet without hope our existence is darker. Hope must be nurtured and cultivated. It fosters our resilience and efforts to move forward, the sunshine for our soul.
What are you hoping for?
This is not the time to be passive; it’s the time to start forming the vision for your future. We cannot change the past; it shaped us. Yet we can dream and plan for how we would like our future to unfold. Hope comes from our soul and it is the second chance we have to reshape our future.
It’s not a solo act
Hardships and challenges are made lighter when shared! Now more so than ever isolation and loneliness are crushing hope. Nurture old and forgotten acquaintances; cultivate new friendships and relationships, to provide you with that comforting wrap that reminds you that you are not alone. Unfortunately, these days, personal meetings are discouraged. If video communication is not your style, go back to the basics with calls, cards, and letters. Take some action, reach out, and “touch” another person, it favorably impacts both of you.
Caregiver’s Hope: It’s Not a Four-Letter Word
The challenges of caregiving can be daunting. Caregiving tasks and responsibilities often increase as our loved ones decline. Many caregivers wish for their loved ones to be fully “restored.” Unfortunately, that is not a realistic hope.
Dealing with caregiving with physical distancing and fear of COVID is making life tougher. Focus on the small positives of the day, the small unexpected things that brought a smile to your face. Engage in something you may not have expected to master. Perform an act of kindness; brighten the day for someone else.

Cultivate Hope: The Survival Plan
- Write about your feelings, wishes, and hopes for the future
- Create a routine that involves communicating with others
- Perform a daily act of kindness for (send a note, do a chore, make a call) for others, and hopefully soon that will include a personal visit
- Engage in a hobby, listen to music, read, pray, paint, knit, work on a puzzle or game
- Take a free educational course on-line
- Find something to laugh about
- Exercise
- Do something nice for yourself each and every day!
Hope like love, is a four letter word
Resources:

Many people are asking about how to celebrate while warring with COVID-19. The reality is that this year familiar ways of celebrating will be different. For many it will be an essentially “virtual” experience, augmented by what can be safely shared or delivered. The war is against an invisible enemy that unfortunately some still do not recognize. This enemy has targets; seniors, those with chronic conditions, compromised immunity, obesity, and then there are those who we would least expect to succumb to COVID-19. You must celebrate while waging war against COVID-19.
How to celebrate, while waging war?
This is the time to celebrate while waging war COVID-19; be creative and consider which traditions can still be safely observed unchanged. “Safe” traditions may include: home decorating, sending cards, listening to music, baking, and making calls to friends. Then move to those that can be observed with minor modifications. Shift to online holiday purchasing, send a check or gift card, or send a food basket instead of the homemade goodies. Virtual gatherings will replace holiday parties; be sure to get dressed up and do something special for these gatherings. Recognize that the traditional get-togethers of friends and family will have to wait; consider how you will celebrate in the future.

Celebrate no matter what!
Traditions anchor us. They are links to our past and those we cherish. Fight COVID-19 with some joy and cheer. No matter what is going on, take time to reflect on the meaning of the season. Celebrate your traditions while waging war with COVID-19. This may be the right time to start some new traditions. Chat with others to explore how they are making modifications, you might get a great idea to include in your holiday observance.
This year be creative and safely observe meaningful traditions. Be sure to reach out to someone who could benefit from some support, good cheer, and acknowledgment.
May your holiday be bright, cheerful, and full of gratitude.

Resources

Thanksgiving 2020: a time to flip the perspective. Despite all the difficulties that we or our loved ones experienced this year, the search for something to be thankful and grateful for may be more challenging at this Thanksgiving. Many are taking note of the public health warning, placing health and safety first protecting their loved ones and themselves from COVID-19 exposure. This is the time to create a new, “one-off” way of celebrating, and hopefully next year we can all resume our traditional Thanksgiving celebrations.
Thanksgiving 2020: Flip The Perspective
Now, on the eve of Thanksgiving 2020: a time to flip the perspective, reflect back, and articulate all those expressions you made while stressed and preparing for the large gatherings. They may include comments similar to these, add your own, be sure to smile and share.
No need to:
- Start preparing a week in advance
- Bake four desserts
- Make extra side dishes for those with special dietary needs
- Clean the whole house
- Listen to the “crazy” relative or friend who always disagrees with everyone
- Feeling obligated to taste everything
- Be saddled by left-overs
- Buy hostess gifts

Thanksgiving 2020: Flip the Perspective and Make It Special
This is the year for the intimate celebration, with those you live with. Despite the hardships reflect on and share some of the kindness you experienced. It could be as simple as gratitude for calls, Zoom sessions, a meal being dropped off, or a friend helping out when things seemed bleak. Make your mealtime festive. Use a table cloth or special table mat; add a candle or two, take out the “good china” and cutlery. If there has been an item that traditionally has graced your Thanksgiving table, put it on display. For some it may be the pilgrim shaped salt and pepper shakers, for others a platter or cranberry dish. Do something different to bring a bit of extra joy to your meal.
Bring Joy to Others
Although this year our gatherings are intimate, there are those who will be alone. These family members and friends need an extra dose of love. Let them know how much they mean to you. What to do?
- Phone or Zoom
- Drop a package at their doorstep
- Send a surprise gift of food, flowers or an item you know that they would enjoy
- Arrange for something helpful to be done for them
Thanksgiving 2020 – Thankfulness
- Reach out to someone outside your home
- Do something that you will be glad you did later
- Do something just because you want to
- Get in at least one good laugh
Wishing you a relaxing and stress free Thanksgiving 2020.
Resources
Why Many Caregivers and Care Recipients Are Feeling the Holiday Blues

Are you an individual or a couple with no children, siblings, partner, or family? Then you are an elder orphan or solo ager. Are you aging alone, without immediately available family, or relatives who live too far away to be helpful at the time of crisis, is challenging? Are you estranged from your family? The terms childless boomer, elder orphan, and solo ager describe those without an aging supporter. Aging can’t be denied, so plan for your future with open eyes.
Who Will Help You?
Navigating major life decision making is difficult when you are alone, sick or incapacitated, physically or mentally. Elder orphans and solo agers need to plan; considering who will step up to provide practical, physical, and emotional support over time. You may recognize that there is no one in your network at present who can take on this responsibility.
You may have planned on moving into a senior community to take advantage of the social, and cultural activities. Given the pandemic, your decision to move may be on hold. Now is all the more reason to ensure that you have a viable solo aging plan in place. Should you need placement, take the time to consider your options, review your finances, and health status, identify your preferences, and consider getting on a waiting list or two. Realize that your first placement choice may not able available when you truly need it. Back up options are necessities.
There are sobering times that force you to examine the options earlier than anticipated. Consider who will care for you if you break a hip, or have major surgery. Would you be able to navigate a wheelchair or walker in your current bathroom or kitchen? Would friends be able to bring meals and provide support? The pandemic has forced many individuals to reconsider their aging-in-place plans. How does the current reality impact your plans?
AARP has many wonderful downloadable resources in multiple languages to help guide you in developing your personalized plan. Additionally, there are guides for the military and LGBT community. Prepare to Care: A Caregiving Planning Guide for Families
Buddy Systems
Individuals with “relationships” tend to age better and are happier in the process. Find like-minded individuals. Connect with other elder and solo agers, form your own support and networking group. Call, or video chat to maintain engagement. This is the time to grow your social network, strengthen your ties with family and friends. Facebook has a private Elder Orphans’ group with over 9K members, a mechanism to learn from the experiences of others. There are also a number of other elder orphan groups with a religious or community focus. Home health agencies are focusing on serving this market, and developing unique programs to engage and share their services, helping individuals’ age-in-place.
Who Will Speak For You?
Don’t leave your decision making needs to chance! Who will serve as your spokesperson, advocate, and ensure that your wishes and preferences will be respected? Have you completed your Advance Directives? These documents are state-specific and may include a living will, durable power of attorney for both healthcare and financial decision making and a Do Not Resuscitate order (DNR). It is important that you discuss in detail your preferences, and validate that the individual you selected to speak on your behalf when you are unable to do so, will respect and abide by your wishes.
Options for Solo Agers
If you do not want to obligate a friend or family member to act on your behalf, or there is no one you feel connected to that your feel would respect your wishes, don’t despair. There are professionals who can assist you in ensuring that that your again plan will be honored. Word of mouth is a place to start and then speak with trusted professionals to find the right advocate for your specific needs.
- Elder attorney
- Certified Financial Planner
- Geriatric Care Manager/ Aging Life Care Professional
- Professional caregiver/companion
- Senior placement agencies
Living Arrangement for Elder Orphans
Most individuals in the United States want to age at home. This involves ensuring that your home has been modified to meet your changing physical needs. Have you consulted a physical or occupational therapist that can provide recommendations based on your specific medical needs? Consulting a professional is especially important when you have a chronic illness, they can help you in making the most appropriate home modifications.
What happens when you can no longer safely remain at home? Have you placed yourself on a waiting list for a Continuing Care Community (CCC), group home, or nursing facility? Individuals are joining forces together to come up with creative living situations. Some are buying homes together, making gaining-in-place modifications and creating some joint spaces for meal sharing and socialization.
Transportation for Solo Agers
If you are no longer driving, how will you get around? Is a ride service right for you, is it available around the clock to meet your needs? Consider your geographic location, weather, and the amount of assistance that you need to get around. The cost of insurance and car maintenance may far exceed the cost of a ride service. As we age, our reaction time and speed of thought diminishes. Consider the safety factor of letting someone else drive you to your destination.

Action Plan for Elder Orphans
- What’s your safety net?
- Consider what your best aging plan is. Who do you need to engage to formalize and ensure that your wishes will be honored
- Advance directives documents reflect your current wishes, are up-to-date, and copies provided to the individuals who are your healthcare and financial power of attorney
- A financial plan meets your aging choices
- What are you going to do to develop new friendships and relationships as you age?
- How are you going to keep your mind active?
- Declutter – donate or discard items that no longer bring you joy and pose a trip or slip hazard. Designate how other items are to be managed in the future

Resources
Solo Agers: Everyone Needs a Support System
Elder Orphans: How to Plan for Aging Without a Family Caregiver
Will My Advance Directive Be Followed?

Anticipatory grief is the set of feelings associated with an impending loss. Anticipatory grief: the space between what happens when a death is expected, but before it actually happens. It can last for a long time, especially when caring for a loved one with a chronic illness. Caregivers, family members, and friends recognize the decline in the loved one condition and the associated loss and change in the relationship. Change in itself can produce anxiety, worry, and anticipatory grief just from fear of the “unknown.”
Who Else Experiences This?
Many loved ones, especially those who are alert and oriented, realize that they are in a declining physical state and experience anticipatory grief. They perceive a lost sense of self-value and worth and often express that they feeling like a “burden” to family.
Your loved one may be worried about you, as much as you are worrying about them. Common concerns relate to how the survivors will manage their daily routine, and who will take over those activities and responsibilities that the loved one usually performed. Often, they think about and may even express thoughts relating to:
- Expectations in the coming days
- Worrying about getting you through this time
- Concerns about care and comfort measures
Using Anticipatory Grief
Anticipatory grief can help caregivers, family members, and friends prepare emotionally for the loss. It can be a time to take care of unfinished business with the loved one, sharing final thoughts such as saying “I love you” or “I forgive you.”
Anticipatory grief involves mental, emotional, cultural, and social responses. Each individual responds uniquely. Symptoms of anticipatory grief may include the following:
- Depression
- Feeling a greater than usual concern for the loved one
- Imagining what the loved one’s death will be like
- Preparing emotionally for what will happen after the death
Does Everyone Experience Anticipatory Grief?
Not everyone experiences anticipatory grief. Caregivers, Family, and friends of the loved one trying to accept the future loss may make it seem that the one dying has been abandoned. Grief experienced before death does not lessen the grief experienced after death or shorten the grief duration.

Dealing with Anticipatory Grief
Feelings of depression, anxiety, or discomfort are normal, when they interfere with the ability to carry out routine activities or cope, then obtaining assistance in addressing those feelings is important. Supportive counseling can be obtained from clergy, hospice entities, social workers, or mental health counselors. Culture and religion can influence how individuals address anticipatory grief.
Action Steps
- Acknowledge your feelings
- Journal. Write about your feelings so you can reflect and notice how they change over time. Focus on including things that went well that day, pleasant surprises no matter how small they may be
- Take time to recharge. Do something that will bring you some pleasure; listen to music, take a bath, exercise, sit quietly with a book. Remember that you cannot care for someone else when you are “running on empty.”
Resources
Medical Definition of Anticipatory grief
Anticipatory Grief: Preparing for a Loved One’s End of Life
SAMHSA’s (Treatment Referral Routing Service) National Helpline, 1-800-662-HELP (4357), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders. This service (part of HHS) provides referrals to local treatment facilities, support groups, and community-based organizations. SAMHSA’s
Traditionally, this is the time of year that everyone is reminded to get the flu shot. Today, flu and COVID-19: a dicey combination. Most of our lives changed significantly around March 2020. Many of us thought, and hoped that COVID-19 would be a thing of the past by now. Yet it is vital that each of us is prepared for the upcoming flu and COVID-19 combination season.
A significant number of high-risk individuals have already felt the impact of COVID-19; especially those in facilities, and in the high-risk groups. With college students returning from campuses, younger children in daycare settings, and some children attending school in-person, the risks of flu and COVID-19, the dicey combination, have been magnified.
Flu Shot
COVID-19 has helped shed light on the importance of social distancing, and mask use to minimize spreading. Protection against the flu is available and strongly encouraged for everyone 6 months and older with no contraindications, by the end of October. This is a very important step that you can take to decrease the chance of getting the flu. This year’s flu shot composition includes updates to the following strains:
- Influenza A(H1N1)pdm09
- Influenza A(H3N2)
- Influenza B/Victoria lineage components
The CDC recommendations also include information on two new vaccines designed to achieve a stronger immune response in people 65 and over.
Will a flu vaccine protect me against COVID-19?
“Getting a flu vaccine will not protect against COVID-19; however flu vaccination has many other important benefits. Flu vaccines have been shown to reduce the risk of flu illness, hospitalization, and death. Getting a flu vaccine this fall will be more important than ever, not only to reduce your risk from flu but also to help conserve potentially scarce health care resources.[i]”
Preparing for Flu Season
Vaccine makers are increasing flu vaccine production this year to meet the anticipated demand. The CDC is launching a nationwide flu shot campaign, encouraging more Americans to get vaccinated. Pharmacies, hospitals, and providers are setting up tents in parking lots, administering the vaccines curbside, or requiring patients to make an appointment to manage volumes.
Action Steps
- Schedule your flu vaccine – appointments are especially important this year given social distancing requirements, and that fact that many individuals are not getting the vaccine at work or school
- Flu shots are covered by most insurances
- Check with your healthcare provider, pharmacy, supermarket, community center, health department, local hospital
- Free flu shots are available in many communities – check with your local health department
- Keep wearing your mask and washing your hands often
Caregivers, remember that your loved one relies on you to be there for care and support. Don’t get caught in the Flu and COVID-19: a dicey combination. Get vaccinated!
Resources
CDC shares flu shot recommendations for 2020-21 season
Beset by Coronavirus, Health Authorities Brace for Flu Season
Social Distancing Isn’t Isolation
[i] Frequently Asked Influenza (Flu) Questions: 2020-2021 Season

Grief is a reaction to a major loss. Your grief journey is unique; meaning that each person navigates the journey on their own timeline, and in their own way. No two people have the same grief experience. Your grief journey, is without a roadmap, is shaped by many factors including the nature of your relationship with the loved one (where you close or at odds), the circumstances associated with the death (tragic, unanticipated, or after a prolonged illness), and age of the one who died are just some of the factors that can impact grieving.
Your grief journey is unique, what you experienced in the past may be very different from the one you are currently experiencing. Consider the loss of an aged chronically ill parent with whom you were very close, against the sudden loss of a child, under tragic circumstances. Both of these are profound losses, yet your reaction to each of these deaths, and the associated grief journey will be different.
Your Grief Journey
No one can tell you how to grieve or feel! Your religion and culture may provide a framework of rituals and customs that can be helpful in addressing mourning and grieving. Never forget that as individuals the grief journey is your own; remember we all heal at a different rate. Mourn; express your feelings and thoughts relating to your loss. Become acquainted with your pain of loss, and notice how the feelings change over time. Take note of the physical symptoms (anger, guilt, anxiety, despair, difficulty sleeping, changes in physical health) you experience on your grief journey; over time they should begin to lessen.
Your relationship with the one who died was unique. What you shared together, the good and not so good, is different from the relationship that individual had with others. Your relationship, the life lived by your loved one, circumstances relating to the death, and other issues that you were facing at the time all impact the grief journey.

Be Ready
Family and friends often mean well, yet the remarks of those who have not been through a grieving journey can appear insensitive. Too often those that do not know what to say, are uncomfortable in the situation and say something without truly considering the impact on you. Such comments include “get on with it”, “keep your chin up”, “It’s been six months you should be over it now” are just a sample of what you may hear. As my mother-in-law said “God gave you two years, one for the comments to come in and the other for them to go out.” Don’t get trapped in these remarks. Others may be seeking details relating to the circumstances of the death that you are uncomfortable sharing. This is your time for remembering your loved one in your special way and beginning to adjust to your new “normal.”
Statistics
The National Center for Biotechnology Information (US National Library of Medicine) notes that unresolved grief can result in a number of issues, up to 1/3 of individuals will encounter physical or mental health effects, or both. A quarter of those who have lost a spouse will experience clinical depression and anxiety. These findings indicate that you are not alone in struggling with unresolved grief, and a reminder that there are many resources available to assist you in navigating your grief journey.
Action Steps
Action Steps means that assistance in dealing with grief is a recognized necessity. One should not struggle alone in dealing with grief. There are many trusted resources available to assist your on navigating your grieve journey.
- Seek assistance from a healthcare provider or spiritual leader (mental health provider, clergy, bereavement counselor)
- If your loved one died while under hospice care, there are bereavement services that you may be entitled to
- Join a support group (community centers, religious organizations, hospices)
- Journal your feelings and emotions
- Avoid isolation, find something that connects and grounds you
- Accept help
- Take care of yourself
- Embrace your loved one and channel your energies! Consider dedicating your energies to an organization related to your loved one’s illness, cause of death, or suicide prevention (1-800-273-8255)
- Begin designing your new future

Final Thoughts
The grief journey is personal providing you to come to terms with your loss on your timeline. As you navigate through the challenges of grief, remember that there will be brighter days to look forward to in the future. Over time, the highs and lows of emotions will be less steep. Take advantage of those who are offering true assistance, and also consider how your loved one would want you to move forward.
Resources
Grief and Loss Includes a list of links to organizations helping individuals with various types of grief journeys
Helping Someone Grieving– What Should I Do?
#grief #caregiving #seniors

The award winning words of Pittsburgh’s Gerald Stern poem “Lucky Life”, serve as a balm for caregivers. “Lucky Life” is a gentle reminder that life is made up of so many different experiences. Caregivers and “Lucky Life” have so much in common, despite painful times, once can reflect back, and find joy and gratitude in life’s experiences. Pain surfaces periodically, reminding us to savor the sweeter moments that life has provided, the memories of those times that should re-anchor, and rejuvenate us.
Stress Relief with “Lucky Life”
Caregivers need to find relief from stress! Capturing the feeling of joy and pleasure at the beach is one such memory. Taking in the feelings at water’s edge, the reenergizing sensation needed for sustenance. The cleaning sensation, or relief from pain, reminding us that life is made up of so many different feelings and memories.
Take a few minutes to read the captivating words of Gerald Stern, and then listen to him read them. Consider reading this to your loved one, and savoring the moments of reflection.
Lucky Life
“Lucky Life isn’t one long string of horrors
and there are moments of peace and of pleasure as I lie in between the blows.
Lucky I don’t have to wake up in Philipsburg, New Jersey,
on the hill overlooking Union Square or the hill overlooking
Kuebler Brewery or the hill overlooking S.S. Philip and James
but have my own hills and my own vistas to come back to.
Each year I go down to the island I add
one more year to the darkness;
and though I sit up with dear friends
trying to separate one year from the other,
this one from the last, that one from the former,
another from another,
after a while they all get lumped together,
the year we walked to Holgate,
the year our shoes got washed away,
the year it rained,
the year my tooth brought misery to us all.
This year was a crisis. I knew it when we pulled
the car onto the sand and looked for the key.
I knew it when we walked up the outside steps
and opened the hot icebox and began the struggle
with swollen drawers and I knew it when we laid out
the sheets and separated the clothes into piles
and I knew it when we made our first rush onto
the beach and I knew it when we finally sat
on the porch with coffee cups shaking in our hands.
My dream is I’m walking through Phillipsburg, New Jersey,
and I’m lost on South Main Street. I am trying to tell,
by memory, which statue of Christopher Columbus
I have to look for, the one with him slumped over
and lost in weariness or the one with him
vaguely guiding the way with a cross and a globe in
one hand and a compass in the other.
My dream is I’m in the Eagle Hotel on Chamber Street
sitting at the oak bar, listening to two
obese veterans discussing Hawaii in 1942,
and reading the funny signs over the bottles.
My dream is I sleep upstairs over the honey locust
and sit on the side porch overlooking the stone culvert
with a whole new set of friends, mostly old and humorless.
Dear waves, what will you do for me this year?
Will you drown out my scream?
Will you let me rise through the fog?
Will you fill me with that old salt feeling?
Will you let me take my long steps in the cold sand?
Will you let me lie on the white bedspread and study
the black clouds with the blue holes in them?
Will you let me see the rusty trees and the old monoplanes one more year?
Will you still let me draw my sacred figures
and move the kites and the birds around with my dark mind?
Lucky life is like this. Lucky there is an ocean to come to.
Lucky you can judge yourself in this water.
Lucky the waves are cold enough to wash out the meanness.
Lucky you can be purified over and over again.
Lucky there is the same cleanliness for everyone.
Lucky life is like that. Lucky life. Oh lucky life.
Oh lucky lucky life. Lucky life.”
– Gerald Stern
Closing Thought
Remember that life is not always painful; the importance of reminiscing about the good, and happy times is vital. Luck is tied to our surprise that the universe can still bring moments of joy, pleasure, and peace amid the challenges of caregiving, and grief. Take time to refocus, refresh, and embrace life fully, again, and again.
Resources
Lucky Life – Gerald Stern Reading his poem
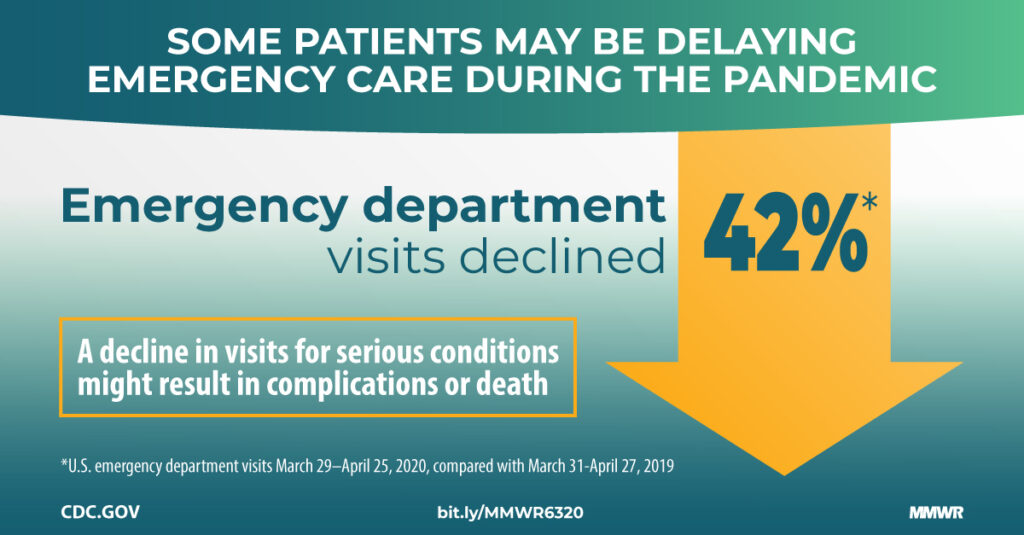
Health conditions and sudden symptoms don’t break for COVID-19. The impact of COVID-19 is being felt in every aspect of life. It has changed how we shop, pray, eat, socialize, and seek medical care. Many of us are thinking twice, or even three times before seeking medical care. The fear of contracting COVID-19, on top of a current medical issue is a sobering thought. Are you one of the 30-50% of Americans that is delaying care?
Chronic health conditions and sudden symptoms don’t break for COVID-19! The real question is “what is going to happen if I don’t seek the needed chronic monitoring or emergency care?” Delaying accessing, care can mean that your symptoms progress, and will be more difficult to treat, or there may be some type of permanent impact of not obtaining care in a timely fashion.
What to Do During COVID-19?
Chronic Care Monitoring
Management of chronic conditions (like diabetes, heart disease, and COPD) and immunizations should not be deferred. Early identification of a change in condition, along with appropriate management can minimize the recovery time. Keeping chronic conditions in check is one less worry.
Time-Sensitive Diagnostic Test
Colonoscopies and mammograms are examples of screenings that can detect a number of medical conditions, some of which are serious. Check with your practitioner about any specific concerns relating to the timing of your diagnostic testing.
Sudden Symptom Emergency Care
In a medical emergency, every minute counts. Sudden onset of symptoms of a heart attack, stroke, dental emergencies, severe abdominal pain, and treatment for certain cancers must not be ignored. Whenever possible, discuss your situation with your healthcare provider. During the conversation, provide detailed information, be clear in your description of your symptoms, and answer questions as candidly as possible. Be sure to mention the “when, where and what” of your symptoms; if there is anything that makes it better or worse, and be sure to share all medication taken (prescription, and over the counter). Telehealth options may be available, and could assist in the management of your situation.
Take Action
Staying healthy is vital; don’t delay getting time-sensitive medical care, or ignore a sudden change in condition. Addressing changes in medical conditions early and promptly responding to a medical emergency improves your outcome. This is especially important if you are the caregiver, and your loved one is depending on you. Look after both your mental and physical health; be sure to do something nice for yourself each day.
Resources
Framework for Healthcare Systems Providing Non-COVID-19 Clinical Care During the COVID-19 Pandemic
Emergency Medical Care – VA Care
Patients are still delaying essential care out of fear of coronavirus

Caregivers healing with the power of art can be a strong way to cope with the stresses of caregiving. During these times, we may find ourselves more isolated in the relationship with the person we are caring for.
- What are simple ways to create beauty in open spaces surrounding us, as we care for others?
- How can we create a healing environment by simply bringing the beauty of light, art, music, and flowers?
The energy we create can be positive or negative. What we hold in our heart matters. Caring for ourselves is essential, and how we feel in our emotions and in our bodies is part of creating love inside the intimate space of caregiving. Caregivers healing with the power of arts is transformational.
Creative Energy
The sharing of creative energy during caregiving can be as simple as reading your favorite poetry, or stories. The power of voice can be soothing, and healing; using the voice to calm both ourselves, and our loved one. Singing softly and playing music is so sweet, and relaxing.
Pause and consider…. As we care for our loved ones we can ask ourselves:
- What are we also deeply passionate about?
- What is something we can share of ourselves?
This is a very special time to do something together with our loved one. Sometimes just being quiet, and present is all we need to do. Listen to our loved one’s favorite music, and ask them about their favorite memories!!!
Or simply listen to your favorite music, dance in your living room, sing your favorite songs with the person you are caring for.
Sharing the Energy
Feeling your own joy can activate the power of the healing potential inside this moment of transformation. We change inside the process of caregiving, no one else can go as deep as we feel, as we care take another human being. We are hyper alert and sensitive. There is a deepening of our own humanity.
The most powerful gift you can share with someone is your authentic presence, and your expression of your being there.
Transforming the Energy
If we create the opportunity to make art, it is by its very nature: transformational. Creativity takes on many forms of expression. Spend time speaking to your loved one, fill in the gaps about their life and of the family history.
- Tell me your life story?
- What were your favorite places you ever visited?
This may be a beautiful opportunity to form an oral history, and a journal of old photos and letters. Having your loved one sit and be present with you, while you garden, cook, paint, or create poetry is connecting. It may be a time for you to tell your own stories, especially if your loved one is unable to communicate.
Self-Reflection
While I cared for my grandmother, she was confused and demented. She spoke to me about loss, memories, and hidden family secrets. I would sit beside her and listen to her descend back into the past. Tell me more….. I would memorize her fragmented stories as I walked along with her into the fogged past. I sat beside her and stretched drawings. I painted her memories, and I fell in love with her in a new and different way. I discovered her in a totally new way. She talked to her mother, and I listened. I could feel her experiences. I realized more about the lost passages of her life.
I painted the Grandmother series in my grief.

Everyone is an Artist
Life is an expression of being. Everyone has inner resources to heal deeply. This involves a journey to discover your inner creativity. You may surprise yourself, and fall in love with your creative expression. You feel, and discover an impulse of freedom to create!
Resources for you to begin your personal journey of making art!
Healing with the Arts is a Free Online course that can inspire and ignite your creativity. It has 6 modules to demonstrate fun activities to explore. What feels good, push pass the inner critic and try something new and different?

I am grateful to the author of this blog post, Mary Rockwood Lane, Ph.D., RN, FAAN for sharing and encouraging caregivers to take advantage of the power of healing through art. Mary is a professor, painter, and nurse. Co-founder and co-director of the Arts in Medicine program at the University of Florida. She has published many articles on nursing and medical journals on healing through art.

Caregiving is stressful and challenging, that’s an understatement. Caregiving in the midst of hurricane season adds new challenges and reminds us of the need to preplan. Preplanning can reduce your frenzy when a hurricane is looming in your area. Hurricane season begins on June 1st and ends on November 30th; unfortunately, Mother Nature does not abide by a calendar, with storms occasionally falling outside of the typical season.
The 2020 hurricane season is predicted to be a busier than normal season; as such, caregiving in the midst of hurricane season will require a bit more foresight and preparation. COVID-19 has added a few challenges to hurricane preparedness. Social distancing, reduced in-person shopping hours, and product availability have resulted in delayed or incomplete hurricane preparedness.

Being Prepared
Successful and less stressed caregiving in the midst of hurricane season requires thoughtful preparation. Consider your personal situation; mobility limitations, dependence on medical equipment, need for professional caregivers, and the probability of flooding and evacuation. Reflect back on your previous hurricane preparedness experiences, what went well and what do you need to differently to prepare this year? Realize that caregiving needs may have intensified, and dependence on paid caregiving assistance may have grown. Consider your ability to manage without paid caregivers and what you can do to ease your caregiving burden before the storm strikes.
Given the current COVID-19 pandemic, the importance of early preparations cannot be understated. Plan to be able to manage for 14 days, with the very real possibility of the loss of electrical power and water. Last minute planning will leave you without necessary supplies, and the real possibility that you may not be able to obtain regularly needed caregiving assistance and support.
Special Needs
For those living in their own home with a loved one with special medical needs, contact and register with your local fire department and/or office of emergency services for special assistance before a storm is forecasted. This is especially important for those who have power dependent medical equipment. Preregister for space at a medical shelter; these facilities typically are set up with backup power to meet the needs of individuals with extensive care needs. Preregistration is critical to ensure that they can meet your loved one’s needs. Those with a loved one who uses continuous oxygen should touch base with their vendor to ensure that they will have sufficient back up oxygen, and are able to open the backup tanks.
Alzheimer’s & Dementia Considerations
Additional considerations are needed for those with Alzheimer’s and dementia. The disruption in routine and potentially setting can trigger behavioral changes. Enroll in MedicAlert® + Alzheimer’s Association Safe Return®, a 24-hour nationwide emergency response service for individuals with Alzheimer’s or related dementia that wander or who have a medical emergency. Call toll-free at 1.888.572.8566 or visit Alzheimer’s Association. If you are already enrolled in MedicAlert + Safe Return, make sure your information is current.
Home Health/Hospice/Professional Caregivers
These individuals are your key support system, check in with them to discuss your personal situation. Be ready to review with them the need for additional medications and supplies to get through the storm; accounting for potential delivery disruption. If you need to leave your residence, be sure that they know where you will be, and how you can be reached.
Food
- Bottled water – at least one gallon per person, per day. Additional water may be needed for food preparation and sanitation.
- Nonperishable food – consider what you will eat with the loss of refrigeration or water. This is especially important if there are dietary restrictions or special needs. Canned goods and prepackaged items, jam, peanut butter, prewashed fruits and vegetables, dried fruits, protein bars, etc. Don’t forget the hand operated can opener.
Utility Interruptions:
The typical inclination to light candles when there is a power interruption is a safety hazard when oxygen is in use. You will need to rely on flashlights for illumination.
- Keep “reusable” ice packs in the freezer. Fill empty spaces in your freezer with plastic container of water, this will help to keep frozen food items cold for a longer time should there be a power loss.
- Once the storm is announced, begin freezing extra ice cubes for the use in coolers.
- Locate and charge battery operated equipment (fans, flashlights, cell phones, radios, medical devices, etc.) gather batteries for use in non-chargeable flashlights, etc.
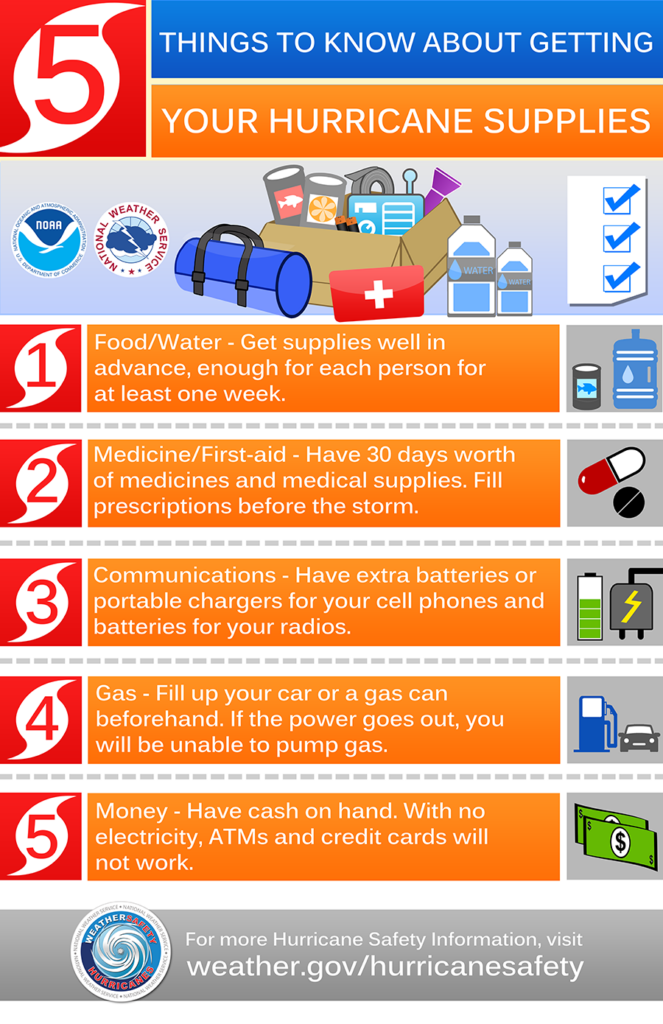
Medications, Medical Supplies and Equipment
Ensuring that you have an adequate supply of those critical items, including incontinence products needed to keep you loved one comfortable. Pack items in plastic resalable bags, to minimize the change of packaging getting wet or torn if evacuation is necessary. Label bags with your loved one’s name, in the event of evacuation the contents can be returned to you.
Don’t leave anything to chance, have at least the two week supply of prescription medications (including the ones used occasionally and a vital to keeping your loved one comfortable), supplies, and any needed back up equipment. Minimize the chances of being caught off guard, COVID-19 back log issues and storm related disruptions means medications and supplies are not always making it to store shelves on time.
Social Connections
During times of illness and crisis, social connections take on even greater importance. None of us can survive caregiving without support. Think of how nice it is to get that unexpected call, checking to see how you are doing with an associated genuine offer of specific assistance. As you are preparing for inclement weather, be sure to check with others as to their status and let them know you plans in the event of your need to go to a shelter or evacuate.
Caregiving Support
Consider the sources of assistance that you are currently depending onto assist you with caring for your loved one.Are you utilizing a patch work of care givers? Do you employ private caregiver, services from a personal care or home health agency and/or hospice? Reach out to them as soon as possible to explore what arrangements can be made to assist you ahead of the storm. Realize that given these individual’s personal circumstances, and post storm conditions, the caregiving assistance routine may not be available to you and your loved one.

Sheltering or Evacuation
Whether you are preregistered at a special needs shelter of will be seeking shelter at an emergency shelter, have a plan as to how you are going to get there. Consider your ability to transport your loved one in inclement weather and the need for professional assistance due to the medical needs. Don’t leave anything to chance. Know the location of the nearest emergency shelter.
Pets
Typically, special needs shelters are not able to take pets; plan for how your special friend will be cared for, should you need to leave your home. Have a plan for who will take care of your pet, do not wait to address this as you are evacuating. Check out Preparedness for People with Pets.

Your Checklist
- List of emergency contacts
- List of medical providers
- Copy of Advance Directives
- Recent picture of the person with dementia
- 14 day supply of prescription and over-the-counter medications/occasionally used (constipation, diarrhea, agitation, nausea…), medical supplies, and equipment
- Face masks for yourself and for your loved one (providing the loved one can use the face mask)
- Self-closing bags of various sizes to store medications, important papers, medical supplies, food, easy on/off clothing and other items
- Plastic garbage bags
- Sanitizing wipes
- Incontinence products
- Spare pair of glasses
- Extra hearing aid batteries
- Personal care wipes
- Paper towels
- Manual can opener
- Flashlight, portable radio, batteries
- First aid kit
- Cell phone and (solar) charging kit
- Cash (ATMs may not have power or be filled)
- Evacuation bag with personal hygiene items, good walking shoes, blankets/sleeping bags, travel food, masks, extra pair of glasses, and lists of crucial contacts and medications list.
- Pets – food and water for your pet(s)
Eliminate the burden for yourself, and don’t wait to get the needed supplies and resources in place to a “weathering the storm.” Avoid the last-minute frenzy. Your preplanning foresight will help you focus on the caregiving routine.
Resources
DISASTER PREPAREDNESS, For Seniors By Seniors
Disaster Preparedness for Alzheimer’s Caregivers
Personal Preparedness for Older Adults & Their Caregivers
During these stressful times, it is so easy to focus on what is wrong, what is not going well, and how expectations have changed. I challenge you to look at being happy with what you have. That is a powerful challenge to take on when you feel like all the forces of nature are in opposition. Being happy with what you have, forces you to look at your present situation from a different perspective. Finding joy, and appreciation in places, and situations you may have previously overlooked.
What is Happiness?
Eleanor Roosevelt shared that “Happiness is not a goal; it is a by-product.” Happiness has also been characterized by feelings of contentment and joy. The topic of happiness has been gaining attention in recent month, propelled by individuals expressing frustration, lack of contentment, disappointment, and anxieties at their present situation. Despite challenges of caregiving, trying to carry on as usual, each of us has been impacted by COVID-19. The value of modifying expectations and changing our perspective has great positive mental and physical implications.
Comparisons
According to Dan Gilbert, a happiness expert shares that human beings have the ability to change their view of the world, so that they can feel better about the world in which they find themselves. What are you really paying attention to? Are you comparing yourself against your perceived happiness of others? This provides you with an unrealistic reference point, unduly impacting your happiness. Catch yourself when you are going down the negative “rabbit hole” of social comparisons. Acknowledge that you have the right to be happy; you do not need to be comparing yourself unfavorably to others. Give yourself a dose of self-compassion.
One never knows what is really going on behind the scenes in the lives of others. The version of others that we see may be very different from what is actually going on in their lives. Think how often you try to make your situation in life just a little “rosier” than what it is for the sake of others.
Take a Break
It is time to focus on you and your loved one. Stop the comparisons and savor! Draw out in your mind those happy and pleasurable experiences. Right now, they may seem to be few, and far between, relish them and think about them often. Reflect back on the nice things that others have done for you, and the acts of kindness that you are or have done for others. Be thankful and appreciative for what you do have even when it appears that the world’s forces may be in opposition. Also think back to those life experiences, life cycle events, trips, and other events and experiences that brought you happiness and joy.
“I am the happiest man alive, I have that in me that can convert poverty to riches, adversity to prosperity, and I am more invulnerable than Achilles; fortune hath not one place to hit me.” Sir Thomas Browne, Religio Medici (1642)
Taking Action
You have the freedom to choose to be happy; it is a matter of perspective and focus. Utilize this time to develop habits to support happiness. Be intentional, take action; focus on putting new habits in place, and changing those that are not supporting your happiness efforts. Be intentional in cultivating, and nurturing your positive emotional practices.
- Formally declare that you are going to change your perspective to focus your energies to acknowledge and recognize the positive and things you are grateful for
- Don’t set expectations on a timeline
- Journal – write and reflect on those things, people, experiences that have brought you happiness
- What are the items that bring a smile to your face, what gives meaning to your life? Think about happy memories each day – reflect back on those occasions that have brought your joy
- Stop comparing yourself to others – happiness is not a competition, and comparisons will thwart your personal efforts to increase your happiness.
- Do something for someone else – despite your caregiving tasks, do something for someone else. Making a phone call, sharing a meal, send a card, or simply smiling and acknowledging the presence of someone who may be more challenged than you
- Meditate or pray to refocus your perspective and gain spiritual energy
- Happiness apps – there are many apps available to help you focus on increasing your happiness, a quick search online will help you identify the one that is right for you

Resources
The Surprising Science of Happiness

Has Covid-19 left you frustrated and disappointed? Have there been caregiving, family, or other gatherings that you have not been able to take part in, leaving you with the scene of frustration and disappointment? Frustration and disappointments are an inherent part of caregiving, yet Covid-19 has added new aspects of frustration and disappointment, too often involving lack of caregiving support and companionship.
Daily Caregiving
Daily caregiving has its own challenges that bring frustration and challenges on a regular basis. No matter what ails your loved one, there are good days, and the not-so-good days. Providing and responding to physical care and mental status changes of our loved ones is exhausting. Coupled with the inability to take time for our own personal wellbeing, and recharging, leaves us vulnerable to increased feeling of isolation, disappointment and frustration.
Those around us are wearing masks and other protective items, they can no longer give us a hug and we cannot see their comforting facial expressions. Technology connects us to the outside world, yet at times it misses the mark. Not everyone has access to, or is comfortable with the computer. Software like FaceTime, Skype, and Zoom can help bridge the human interaction gap. However, some individuals are expressing the sense of being “over Zoomed” and find it more stressful to having to “look good” for the other call participants.
Caregiving Challenges
Physical distancing and protective measures resulted in many caregivers having less personal and emotional support for their loved ones. For those living in senior communities, guidelines prevented family member and some paid caregivers from providing assistance. The lack of housekeeping assistance, visits from friends and family also contribute to the sense of isolation. Every caregiver has a story to tell; even in the “normal” times, they found some friends and family became more distant when the loved one’s condition was declining. These feeling for many have been significantly intensified over the last several months.
Disappointed
It is so easy to focus on all that is not going well; the decline of the loved one, the inability to obtain physical caregiving support, not going out to partake in those activities that brought us joy and recharged us. Everyone has had an event that they could not partake in, a funeral, cancelled wedding, anniversary or birthday party, or a celebration of new life that has been put on hold. No doubt the inability to take part in a much anticipated life-cycle event has resulted in sadness. Take a few minutes to grieve those losses, and focus on recharging. No one could have imagined the current state of affairs.
Human Contact
While we are physically distanced from friends and family, we need to make every effort not to be isolated. Are you hungry for human contact? Individuals are social beings, and there is an innate desire for socialization. For caregivers, the need for the additional physical caregiving support and assistance is vital. The need for caregiving assistance and support is more than a quest for sociability.

What to Do?
Given that so much is out of our control, keep your expectations realistic. You can only control yourself. During times of stress, uncertainty, and change, others may act or say things that may be hurtful or disconcerting. This is the time to “give them a break.” Each of us responds to uncertainty in our own way based on our individual experiences and culture. Take a mini mental-break from caregiving responsibilities to focus on YOU!
- Continue physical distancing and taking appropriate precautions
- Try to “connect” in a way that is comforting while being physically distanced
- Do something nice for yourself – consider this the “rainy day”
- Utilize the good china
- Wear something special, just because
- Read a book or listen to music
- Use the fancy soap, or other special cosmetic/after shave that you have been saving
- Destress – consider utilizing a stress reduction app
- Dig into a task that you have been putting off – purging a drawer or file
- Journal
- Express your frustration about your current reality
- Focus on what you have to be grateful for. Document the beauty you see through your window, the random acts of kindness that have been expressed to you. Reflect on happy memories and document them so you can reflect back on them when your mood is dark
- What are you hoping for? What is on your future wish list?
- Create a list, a vision board with pictures – keep focused on the future
- List the people you want to get together with in person – create that visual
- Start to think about how you would like to do when physical distancing guidelines are lifted
- How do you want to “celebrate”?
- What would be meaningful to you?
- Do something special for someone else
- Make a call
- Send a card
- Send a gift that would have meaning for the recipient
- Make a donation to a cause that has meaning to you
This Will Pass
A new normal is on the horizon, things will be different. Yet, there will be opportunities to get back to the things that brought you joy. Think how you will enjoy the many new firsts; getting your haircut, having your nails done, eating out with friends, having additional caregiving support, being able to go to the store and pick out the items you want and not have them picked for you.
Resources
Destress-Stress Management Apps

Becoming a caregiver could come on slowly as a loved one declines or as a surprise, resulting from an accident, sudden new diagnosis, or resulting from unanticipated medical complications. Being thrust into the role of a caregiver often comes without warning or training. Caregiving surprises arise for each and every one of us who has taken on the role of caregiver. If you are a repeat caregiver, your caregiving surprise may be that this loved one’s care is very different from previous caregiving experiences.
On the surface, the role of caregiver appears to helping the loved one in completing the activities of daily living. There are recognized basics of self-care task for maintaining independence: eating, bathing, toileting, dressing, and transferring (functional mobility). One or more of these basic activities have been taken on by the caregiver. This in itself leads to many caregiver surprises. Not every caregiver is comfortable handling such personal care activities and the loved one may be resistant to the needed care and assistance.
You Don’t Know
Each caregiver is unique, as is the loved one they are caring for. Given culture, background, personal, and professional responsibilities, the caregiver may have had little exposure or insight as to what goes into caregiving. You just don’t know what you don’t know! As such, caregiving is a real surprise. One of the first caregiving rules to know is that it is perfectly OK to ask questions and seek guidance. No one turns into a caregiving expert with the tap of a fairy wand.
Each Day, A New Surprise
Caring for a loved one is dynamic; everything is “fluid,” just like a lava lamp. No two hours or two days will be the same, especially as the loved one’s mental and physical health changes. For those caring for a loved one with mental health or dementia issues, the constant repetition of the same question, not remembering simple instructions, or recognizing family members is trying and heartbreaking. Often this is one of the hardest caregiver surprises to muddle through. Having to master ever changing caregiving tasks is straining and results in stress and worry.
Has Anyone Else Done This
Caregiving has been going on since the beginning of time in one form or another. You are not the only person facing caregiver surprises. Combat feelings of inadequacy and isolation by reaching out and asking for specific help and guidance. Guidance, resources, and support are available for the asking; do not be shy about reaching out for assistance.
Do you need help and guidance as to:
- What do I do next?
- How do I take care of “me” while caring for my loved one?
- What does this situation really mean for me, and my loved one?
- Where can I get help?
- Can we stay in our home?
- I have not shared my care preferences and wishes with my children, how do I do that?
- What will happen to my loved one if I am sick in bed?
- What do I tell the family?
- How can I get the family to help me?
- Who do I call about…?
Do these questions sound like those that you have been wondering about? Have you been uncomfortable asking for help and guidance? Assistance and support is available to you, gain confidence and peace of mind. As you embark on this new role, you can minimize the number of caregiving surprises and decrease your learning curve by hiring a consultant to assist you with the caregiving transition.
Resources
Simplifying Complex Care for Older Adults
Ask Me 3: Good Questions for your Good Health
This article was originally written as Care Assistance article/guest blog spot for the Law Offices of Jeffrey G. Marsocci, PLLC.

Memory Creation
Memory creation is impacted by our relationship with our loved one. Each relationship had high and low moments; the real question is how do we want to remember our loved one? After the passing of a loved one, there are numerous options available for preserving precious memories of your time together.
Memory Creation, How To Remember Your Loved One?
For many, the focus will be on happy, and special times shared, while for others, unfortunately, the memories will be centered on feuds, rivalries, and missed opportunities. Memory creation is a way to remember a loved one in a special and tangible way.
Touchable Memories
Memory creation can also be touchable, through various art and media forms. Consider your relationship with your loved one, and what type of a tangible memory form brings meaning to you. There are many different ways to carry out memory creation; to honor, and recognize the relationship that you had with your loved one. There are a number of art forms, and objects that help with memory creation, and serve to keep your loved one’s presence close. Do not be limited by the following options, think about what form of memory creation would bring the most meaning to you.
Pictures, Books and Trinkets
Do you have pictures and digital images of your loved one that brings a smile to your face? Do you have images of places where you spent time together and created fond memories? What about special recognition moments; be they professional or of a family milestone?
Ideas To Consider
There are many services available where digital images of your special pictures can be arranged into a hardcover book containing the images and text that is meaningful to you. You have the flexibility to determine the size and fonts used to highlight the special moments of meaning. This type of a memory book can be created for various family members and friends by utilizing pictures that have special meaning to the recipient.
Photos may also be incorporated into cards, mugs, plates, blankets, tote bags, shirts, and wall hangings. Images etched into wood, Lucite, and glass are gaining popularity. Digital photo albums that continuously display a rotating selection of pictures, is another way to keep the memory of a loved one close at hand.
There are numerous vendors that help you assemble photobooks, some are online, drug store photography departments, and wholesale discount stores.
Memories in Fabric
There is no limit as to how fabrics can take on a special memorial meaning. Imagine how you could remember a loved man who had an extensive tie collection or had a fondness for clothes or fabrics! Consider the creation of a wall hanging, blanket, handbag, or tote bag made up from pieces of ties, shirt cuffs, suits, fancy dresses, lace or T-shirts. There are patterns readily available, or professional services to assist with the creation of a new item made from fabrics that had meaning to the loved one or you.
Pam Missimer, of Baggins Handbags’, is a designer and shares that “handmade bags and other personalized items enhance your beauty and personal style. They are customized and can include a sentimental fabric. By using primarily sustainable and even recycled natural materials like denim and wool clothing, these bags have a unique character while still being versatile and modern. Your sentimental fabric can be turned into something you will use and love every day.”
Many of these craft professionals can be found on Etsy. A quick Internet search will show a variety of examples to help you decide what may be the right memory creation for you.

Jewelry
Your loved one may have bequeathed a piece of jewelry that had meaning to them. Jewelry is very personal, and the item left may not be in keeping with the times or your taste. For example, if your mother or grandmother left you their engagement ring, you could incorporate the gemstones, into a new bracelet or pendant. The new piece of jewelry should bring a smile to your face each time you see and wear it. It is another way to reflect on the special memories that you shared with the loved one. Start by asking trusted friends for recommendations and exploring the work of local jewelers, take your time, be sure that the design is truly what you want.
Plants and Flowers
For some, a garden or a special plant holds a unique connection to a loved one. What was their favorite plant? Cactus, orchids, irises, or lilies may have a special significance to your loved one or you. It may be a hobby that you had in common, or you may have been left with a collection of plants that need some love and attention. This may be a way to create new memories for yourself, while reflecting back on the loved one.
Trees and Stars
For some the connection with the environment is strong, and one way to honor the memory of a loved one is by planting a tree in their memory, the family is typically sent a certificate memorializing the tree purchase. If your loved one was one who appreciated the stars, similar options are available to purchase a star. It is important to remember that this is not an official naming, yet a nice way to honor a loved one. A certificate is also typically sent to recognize the tribute.
Bricks and Plaques
As part of fundraising efforts, many organizations provide a support option that includes purchasing a commemorative brick. The brick or plaques are then engraved with a commemorative message. This provides a visual that can be appreciated by other individuals who frequent the venue.
Individual Memory Creating
Each person’s memory creation is unique to the relationship shared with the loved one. Consider how you would like to create a new memory based on the relationship and love shared. What can you do to help another family member or special friend of a loved one create a tangible memory of distinct times shared? The possibilities for memory creation are endless; let your imagination go wild with the options.
Resources:

Who would have thought that we would be dealing with a pandemic that has impacted every aspect of our lives? Some of us may be quarantined, staying in place, or confused as to what to do. COVID-19 is currently understood to be highly infective and easily transmittable from person to person through droplet and contact spread.
In the near future there is a high probability that we may be one of those who become infected, or we know someone who has been impacted by Covid-19. Hopefully, recovery will be quick, and there will be a return to good health. Regrettably, given the statistics, we will all have the unfortunate opportunity to have someone close to us suffer the more serious impact of this virus, and need hospitalization. This is when it is so critical to have the Advance Directive documentation to guide the medical team as to your wishes. Depending on your age, overall medical condition and availability of resources in your area your Advance Directive becomes more critical.
Care Allocation
The issue of how care resources will be allocated is a hot topic for healthcare professionals and health systems. Care prioritization is no longer a hypothetical, it is becoming a reality. The American healthcare system is quickly learning from China, Italy, Spain and the UK that resources are finite, and will need to be equitably distributed. This is in contrast to the “first come-first served” that some institutions are using. In reality, field medicine (i.e. wars and natural disasters) has been utilizing triage protocols focusing the care on those individuals that had the best chance of making it through the medical crisis.

Dynamic Times
What is known about COVID-19 is being constantly updated. This includes testing measures, management and the handling with the compassion the volume of individuals who are dealing with COVID-19. Individual fears and desires that “everything” be done for your loved one, may not happen. Resources are very limited, and every effort is being made to use them in a way that is fair for everyone. Be prepared that for the fact that despite the best of intentions, not everyone will get all the available resources.
Crisis Standards of Care
Utah’s Crisis Standards of Care Guidelines outlines the allocation of patient care resources during an overwhelming public health emergency. The focus of care shifts to the “thoughtful use of thoughtful use of limited resources for the best possible health outcomes for the population as a whole. Resources are shifted to patients for whom treatment would most likely be lifesaving and whose functional outcome would most likely improve with treatment. Such patients should be given priority over those who would likely die even with treatment and those who would likely survive without treatment.”[i]
Certain preexisting and acute medical conditions may exclude admission or transfer to critical care:
- In a coma or vegetative state; with severe dementia; advanced untreatable neuromuscular disease or other malignant disease
- In end-stage organ failure or failures; or suffering from traumatic brain injury or severe stroke with minimal chance of recovery
- In cardiac arrest; with severe acute trauma; or severe burns with less than a 50% chance of expected survival
- Over 90 years old
New York, Alabama, Minnesota and Tennessee are among the states that also have policies for crisis care. Some of these policies address ventilator allocation[ii]. The Institute of Medicine issued in 2009, Guidance for Establishing Crisis Standards of Care for Use in Disaster Situations, all these resources are guiding, practitioners who have to consider the severity of illness, prognosis, and the amount of resources needed, as they determine how the scare resources are to be allocated. The reality is that practitioners are already making some of these determinations and health systems are working cooperatively to address the allocation of resources in a respectful, ethical and equitable way.

Individuals with Disabilities
The issue of managing the care of individuals with disabilities is challenging given the Federal Americans with Disability Act. Individuals with disabilities are asking the federal government to address care rationing that would deny individuals with disabilities treatment for COVID-19. It will be a balancing act; no matter what, every effort to keep patients comfortable will be made. A recent HHS bulletin notes “Decisions by covered entities concerning whether an individual is a candidate for treatment should be based on an individualized assessment of the patient based on the best available objective medical evidence.”
On April 8, 2020 Alabama removed controversial ventilator guidelines that denied COVID-19 care to the disabled. This was in response to the state’s preparedness plan that prioritized the treatment of able-bodied individuals over people with physical and intellectual disabilities. This was in response to a complaint filed with the Health and Human Services (HHS) Office for Civil Rights (OCR). Allocation of resources is still a critical issue facing front line practitioners, and remains an issue to contend with in these very unusual times.
Palliative Care and Hospice
If there was ever a time to focus on keeping individuals comfortable, this is the time. Palliative care and hospice services are designed to keep individuals comfortable for when aggressive medical care is no longer appropriate. It is the approach of alleviating symptoms and keeping your loved one comfortable. Even if there is no Advance Directive, consider how your loved one would want to be cared for during this crisis. Be realistic recognizing all that is currently known. Would your loved one prefer to pass on peacefully once there is little chance that they will recover? Acknowledge that these are extraordinary times.
Personal Action Plan
- Complete an Advance Directive & upload to a registry – keep it handy and not in a safe deposit box
- Name a healthcare surrogate/proxy
- Ensure your healthcare surrogate/ proxy is aware of the designation and will advocate for you
- Name a backup healthcare surrogate/ proxy is aware of the designation and will advocate for you in the absence of your primary choice
- Avoid probate – contact your elder attorney & financial planner
- Ensure that beneficiaries are named on life insurance policies
- Ensure all property disposition is addressed – there are state specific nuances
- Take the time to communicate with those you love
- Learn more about palliative care and hospice – the symptom management approach for when the underlying condition can no longer be treated
- Reach out to those you have a strained relationship
Stay Safe
- Handwashing
- Social distancing
- Keep contact numbers of family and friends handy
No matter what, kindness, compassion, love, support and understanding must never be rationed!
Resources
CDC Coronavirus 2019 (Covid-19)
Utah Crisis Standard of Care Guidelines
Could COVID-19 force Utah hospitals to prioritize care?
Advanced Care Planning – The Gift of Love
Your Spokesperson – Your Champion
The nightmare of rationing health care
Alabama removes controversial ventilator guidelines that denied coronavirus care to disabled
Minnesota Health Care Considerations – Crisis Standards of Care
[i] Utah Crisis Standards of Care Guidelines. (2019, January 17). Retrieved March 28, 2020, from https://coronavirus.utah.gov/wp-content/uploads/Final_Utah_Crisis_Standards_of_Care_011719-1.pdf
[ii] VENTILATOR ALLOCATION GUIDELINES New York State Task Force on Life and the Law New York State Department of Health. (2015, November). Retrieved March 30, 2020, from
Have you been delaying, or avoiding addressing the topic of Advance Directives? COVID-19 is the Advance Directive jolt, time could be running out. Being a realist, and not an alarmist; I constantly ask the question, what are you waiting for? Who will speak for you, and share your wishes when you are unable to speak for yourself? We are living in unprecedented times, the need for Advance Directives and advanced planning has never been greater. COVID-19 truly is the Advance Directive jolt.
COVID-19 Is The Advance Directive Jolt
The spread of COVID-19 combined with the various national, state and regional responses to treating individuals reinforces the need for individuals to have Advance Directive. Your underlying medical conditions, age, and those you may have come in contact with, may place you at a higher risk for contracting COVID-19. COVID-19 is the Advance Directive jolt. Remove the burden from your loved ones; avoid them having to make decisions without knowing your wishes and preferences. Avoid family members having to deal with your affairs without having all the information to make the best-informed decisions on your behalf.
Resources for Advance Directives
- Elder law attorneys are making themselves available to assist clients during this challenging time. Seek a referral from a trusted friend, relative, or financial planner
- AARP Advance Directive Forms by state
- CDC Advance Care Resources
- Five Wishes available in 26 languages
- Medline Plus, the website of the National Library of Medicine
Peace of Mind
Peace of mind is a gift, not just to yourself but to your loved ones. That peace of mind can only come when you have completed an Advance Directive, named your healthcare surrogate, and spoken to those who you have named to speak on your behalf. These individuals need to be able to pick up and manage your affairs. Have you added these individuals as beneficiaries or granted them access to safe deposit boxes and bank accounts?
Have you shared ALL the information needed to address your business affairs?
- Passwords (banking, websites, insurance, medical portals, utilities, social media…)
- Access to properties – keys for cars, storage units, boats…
- Location of key documents – your filing system, checkbooks
- Provided a copy of your Advance Directive
- Clergy
- Funeral home
Advance Care Planning
There are a number of apps to assist; Just In Case Planning is one free tool that is helpful in organizing all of your Advance Care Planning into one location, and you grant access to those acting on your behalf.
Who would have thought that we would be dealing with a pandemic that has impacted every aspect of our lives? Some of us may be quarantined or staying in place. COVID-19 is the Advance Directive jolt, the kick in the pants to spur action. Utilize this gift of time to address or update your Advance Directive. Take the time to reach out to those you love, let them know how important that they are to you. If you have treasured belongings and know that there is someone who would appreciate the item, tag it or make a distribution of property list. This will minimize some hard feelings down the road.
Relationships
It is also the time to make amends with those you might have drifted away from despite the reason. Make your day and their day by mending the relationship. Leave letters and note for those you care about, share the impact that they have made on you.
The Reality
In the near future, many of us will have been impacted or know someone who has been impacted by COVID-19. Hopefully, we and they will recover quickly, and return to good health. Unfortunately, given the statistics, we will all have the unfortunate opportunity to have someone close to us suffer the more serious impact of this virus and need hospitalization. This is when it is so critical to have the Advance Directive documentation to guide the medical team as to your wishes. Depending on your age, overall medical condition and availability of resources in your area, your Advance Directive becomes more critical.
Personal Action Plan
- Complete an Advance Directive & upload to a registry – keep it handy and NOT in a safe deposit box
- Name a healthcare surrogate/proxy
- Ensure your healthcare surrogate/ proxy is aware of the designation and will advocate for you
- Name a backup healthcare surrogate/ proxy; be sure this individual is aware of the designation and will advocate for you in the absence of your primary choice
- Avoid probate – contact your elder law attorney & financial planner
- Ensure that beneficiaries are named on life insurance policies
- Ensure all property disposition is addressed – there may be state-specific nuances
- Compile a medical and surgical history
- Include all medications, prescription, and over-the-counter
- List all known allergies to medication, foods and any other substance (latex)
- List of treating practitioners
- List emergency contacts
- List the individuals you authorize the practitioners to discuss your care
- Take the time to communicate with those you love
- Reach out to those you have a strained relationship
Stay Safe
- Frequent handwashing
- Practice social distancing
- Stay connected by phone, video chat, email
- Focus on the positive that is going on
- Keep contact numbers of family and friends handy
Resources
CDC Coronavirus 2019 (Covid-19)

Gloves
Have you seen the increase in the number of individuals wearing disposable gloves in public? Gloves do create a barrier between the skin and touched surfaces, but they are only a barrier as strong as the glove. No matter the type of disposable gloves (vinyl, Nitrile, latex) used; gloves are not a substitute for handwashing!
Disposable Gloves
Disposable gloves have been used by healthcare professionals as a barrier to blood and bodily fluids; and became a standard known as Universal Precautions, once it was discovered how HIV was spread. One of the key pieces of information to remember is that gloves are not “perfect”. They may become torn or develop micro-punctures during use that are not easily seen. Gloves wear out. The use of gloves is not a substitute for handwashing.
For the best protection, use the right sized glove. A Cinderella fit is needed; a glove that is “too big” will slide on your hand and make it harder to grip things. A glove that is “too small” may not stretch sufficiently or tear during use. No matter what glove you use, gloves are not a substitute for handwashing. Handwashing should always be done after glove removal.

Putting On Gloves
- Wash your hands well with soap and rinse them with clean, running water. Then dry them well
- Hold the glove (open end) in one hand, and put your other hand into the glove
- Repeat with your other hand
Removing Gloves
There is an art to removing disposable gloves to minimize the chance of spreading germs to yourself and others. When you take gloves off, make sure the outsides of the gloves do not touch your bare hands. Follow these steps: If you are right-handed (if you are left-handed, reverse the steps)
- Grab the open end of your right glove with your left hand
- Pull toward your fingertips. The glove will turn inside out
- Hold onto the empty glove with your left hand
- Put 2 right-hand fingers in the opening of your left glove
- Pull toward your fingertips until you have pulled the glove inside out and off your hand. The right glove will be inside the left glove now
- Throw the gloves away in a waste container
- Wash your hands well with soap and rinse them with clean, running water. Then dry them well
Wearing Gloves In Public
I have watched people using gloves in the supermarket, walking, and while performing a variety of different tasks that do not typically require gloves. The use of gloves can provide a false sense of protection. I have seen individuals with gloves touching their face, and doing things that they would not consider doing without the gloves. Undamaged gloves do offer protection, as long as it is the right type of glove for the job. Do not assume that your gloves are “made of steel” and will never damage. No matter what, gloves are not a substitute for handwashing.
Allergies
Some individuals develop or have allergies to latex (made from rubber). These allergies tend to become more severe with repeated exposure. It is very important that you wash your hands and any bodily surface that may have come in contact with the latex. Monitor your symptoms; seek emergency assistance if you experience any difficulty breathing. Be sure to wear your latex allergy identification bracelet. It is vital that you share this with individuals who may touch you wearing disposable gloves. Verify that latex gloves are not being used in your care.

What To Do
- Seriously consider if you need to use gloves for the task at hand
- Never reuse disposable gloves
- If you have a supply of disposable gloves that could be donated for the care of patients, please do so. Caregivers and healthcare workers do not have the needed supply of gloves
- Wash your hands frequently – gloves are not a substitute for handwashing
Resources
Social Distancing Isn’t Isolation
Social distancing is the new buzz word. According to the CDC, it means “remaining out of congregate settings, avoiding mass gatherings, and maintaining distance (approximately 6 feet or 2 meters) from others when possible.” This guidance is intended to minimize close contact and decrease the chance of coming in contact with someone who has respiratory symptoms. Social distancing isn’t isolation. It does not mean that you have to be locked away from others.

There Are Many Unknowns
Daily, we are learning more about COVID-19, its spread, and the precautions that need to be taken to decrease the chance of exposure. All of the guidance provided relating to COVID-19, also apply to flu protection. The kicker with COVID-19 is that there are many more unknowns; no vaccine and treatments are still being identified. Everyone needs to practice social distancing, to minimize exposure. Social distancing isn’t isolation!
What Is Isolation
According to the CDC, when someone is isolated, they are “known or reasonably believed to be infected with a communicable disease and potentially infectious from those who are not infected to prevent the spread of communicable disease. This lets them recover without spreading the virus to anyone else. Isolation for public health purposes may be voluntary or compelled by federal, state, or local public health order.” Individuals in isolation may, or may not be feeling ill.
Those at Higher Risk
For the elderly and those who are at higher risk of getting sick, often they are already vulnerable to social isolation. The CDC has identified groups of people who are at higher risk and should be practicing social isolation.
- Older adults, over 60, especially men
- People who have serious chronic medical
conditions like:
- Heart disease
- Diabetes
- Lung disease
- People with weakened immune systems
- Those on immune-suppressants and biologics/bio-similars
- Chemotherapy
- Steroids
What You Can Do to Keep Yourself and Your Family Healthy
The most trusted guidance comes from the CDC; their website is continuously being updated, reflecting the most up-to-date information.
- Take everyday preventive actions to stay healthy
- Avoid close contact with people who are sick
- Avoid touching your eyes, nose, and mouth
- Stay home when you are sick
- Cover your cough or sneeze with a tissue, then throw the tissue in the trash
- Clean and disinfect frequently touched objects and surfaces using a regular household cleaning spray or wipe
- Wash your hands often with soap and water for at least 20 seconds
- Wash hands after removing gloves! The use of gloves is not a substitute for handwashing
- Follow public health advice regarding school closures, avoiding crowds and other social distancing measures
- Stay informed. CDC’s COVID-19 Situation Summary will be updated regularly as information becomes available

What to Do if You are At risk
There have been reports of shortages of various paper goods, hand sanitizers, some cleaning supplies, and bottled water. These will be alleviated over time. Do not panic, stocks will be replenished. Be open to swapping supplies with friends and relatives.
- Stock up on supplies (non-perishable food, incontinence, household, supplies, pet supplies, etc.)
- Utilize delivery services for medication, medical supplies, and other items to reduce the number of times needed to leave the home
- Socially distance – Take everyday precautions to keep space between yourself and others
- When you go out in public, keep away from others who are sick, limit close contact, and wash your hands often
- Avoid crowds as much as possible
- Avoid cruise travel and non-essential air travel
- During a COVID-19 outbreak in your community, stay home as much as possible to further reduce your risk of being exposed
How to support those in need
Supporting those in social isolation means ensuring that they have the needed supplies to remain away from the public and still continue with their activities at home. Not everyone has access to commercial delivery services, so the assistance of a trusted relative, caregiver, or friend is so important.
Reach Out & “Touch” Differently
- Provide meals and perishable foods
- Proactively ask what they may need and help them obtain:
- Prescriptions and other medically necessary items
- Hand sanitizer – this may be hard to obtain, many areas are reporting shortages
- Paper goods
- Tissues
- Paper towel
- Toilet paper
- Forms of entertainment
- Library books, audiobooks, magazines
- Puzzles, crossword puzzles, Sudoku books, cards…
- Help them stay connected
- Call and check in on them by phone
- Send greeting cards, or other small items through a mail-order or shipping distributor
- Use of Messenger, Skype, WhatsApp, Zoom
- Mobile assistants, Alexa, Siri
- Determine if professional pet services are needed, if the owner is unable to care for the animal
- Determine if additional services are needed to minimize injury

Stay Connected Safely
To minimize the personal impact of social distancing, be sure the individual is truly not socially isolated. Reach out in a way that is safe for both of you. Be creative in keeping yourself and others engaged and not consistently focused on the various challenges facing all of us today. Use trusted sources of information to guide you through these times.
Resources:

Will My Advance Directive Be Followed?
You have soul-searched and taken the time to think about how you want to live while dying and come to terms with how you would like your dying to be managed. This is not an easy or quick process; for some this journey may take years.
The question “Will my Advance Directive be followed?” This is a real and valid concern that many individuals express apprehension about. Hopefully, you have a healthcare surrogate or proxy who is willing to standby, and advocate on your behalf. The advocacy by the healthcare surrogate or proxy is vital in ensuring that your wishes are honored.
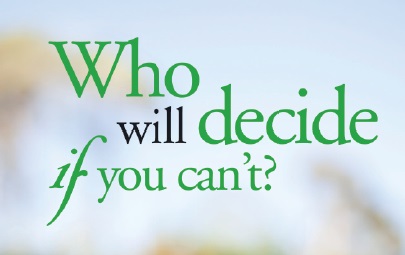
Research Findings
In the recently published article Association of Physician Orders for Life-Sustaining Treatment With ICU Admission Among Patients Hospitalized Near the End of Life in JAMA reported that advance directives entered by physicians, based on the individual’s wishes, were not followed in almost 40% of patients with a terminal illness. Unfortunately, these individuals with chronic life-limiting illnesses who had advance directives, had their wishes were ignored, leading to unwanted aggressive care.
So what does this mean for you? There is no substitute for a healthcare surrogate/healthcare proxy with strong advocacy skills, and a commitment to ensuring that your wishes/values are respected. Your clearly articulated Advance Directive needs to be readily available, and your advocate must be ready to speak up on your behalf.
I have an Advance Directive, Now What?
The Advance Directive is a document that speaks for you when you are not able to share your medical care wishes. It needs to be readily available and visible, to emergency medical responders or caregivers. Your healthcare surrogate or proxy may not be present to alert those that need to know of your wishes, leading to medical care you may not want. The desire to keep Advance Directive documents secure has resulted in them often being place in bank safety deposit boxes, vaults, safes, file cabinets and other secure hiding places making them unavailable in time of need.
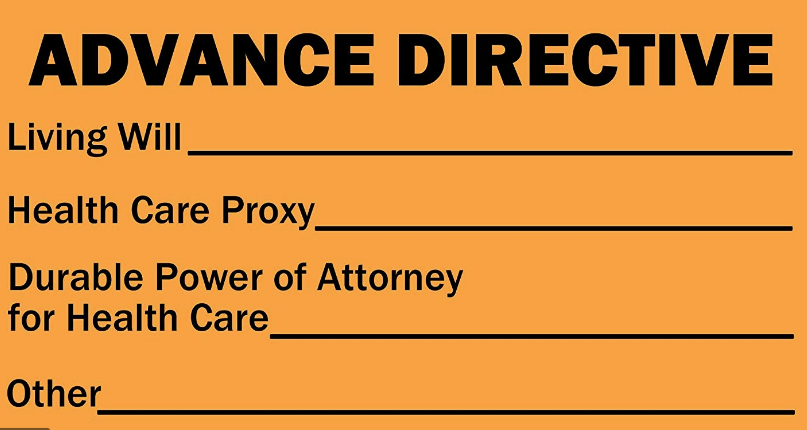
Making my Advance Directive Available
There are a number of registries that provide a platform for you to upload a copy of your advance directive. Some are State-based; others are commercial such as the U.S. Living Will Registry (now known as the Advance Care Plan Registry). These registries make your Advance Directive available around the clock to those with the appropriate access to the information and protect them against theft, fire, flood, or natural disaster. Your healthcare providers should have copies of your Advance Directive, along with your healthcare surrogate or proxy.
Recommendations
Recommendations to ensure that your Advance Directive is available when needed:
- Upload to a registry
- Have several copies available
- Give copies to your surrogate, trusted friends, hospital, and medical providers
- Upload to your phone, and those of trusted individuals who will advocate on your behalf
Take Action
Do not have a false level of security or leave to chance the need for a strong healthcare surrogate or proxy who is informed about your wishes. This individual must have an updated copy of your Advance Directive, be willing, able, and available to advocate on your behalf. For your peace of mind, do not leave anything to chance.
References & Resources
Association of Physician Orders for Life-Sustaining Treatment With ICU Admission Among Patients Hospitalized Near the End of Life. Robert Y. Lee, MD, MS1,2; Lyndia C. Brumback, PhD1,3; Seelwan Sathitratanacheewin, MD1,4; et alWilliam B. Lober, MD, MS1,5,6; Matthew E. Modes, MD, MPP1,2; Ylinne T. Lynch, MD2; Corey I. Ambrose, BSc7; James Sibley, BS1,5,6; Kelly C. Vranas, MD8,9; Donald R. Sullivan, MD, MA, MCR8,9; Ruth A. Engelberg, PhD1,2; J. Randall Curtis, MD, MPH1,2,5,10; Erin K. Kross, MD1,2. JAMA. Published online February 16, 2020. doi:10.1001/jama.2019.22523
Advance Care Planning: Healthcare Directives from the NIH
#advancecareplanning #healthcareproxy #advancedirectives #polst
Just In Case Planning

Do you have a will? Does someone else know your home alarm code? After you are gone, are there items in your home that a loved one might find upsetting? Rather you know it’s coming soon or it feels far off, many people are not prepared for their death.
The new year is a perfect time to take a look at where you’re at when it comes to planning for your “just in case.”
Getting Started
Often, the hardest part of planning is getting started. The free website Just In Case Planning separates your plans into six easy to use forms that you can easily share with loved ones or save to file with other important documents.
Wills and End of Life Care
Wills and decisions about end of life care are probably the topics you would think of first when thinking about planning for “just in case.” However, according to a Gallup poll, only 40% of Americans of all ages report that they have prepared a will.
Setting up advance directives and medical power of attorney is something you may think of as needing only when you are diagnosed with a serious medical issue, but the reality is at any moment your loved ones may have to make decisions that they were not prepared to make. Giving them the confidence that they are making the right decision for you can alleviate so much stress from an already stressful situation.
Funeral Considerations
Everything from burial preference, song choice, and even an obituary can be prepared in advance when it comes to funeral planning. Creating a plan with a funeral home or even writing down your wishes for a loved one can ensure that you are remembered for what matters most to you.
Reflections
Planning for “just in case” can feel administrative and unemotional, taking time to also include letters of reflection to loved ones can be a priceless gift and legacy to leave behind. Just in Case Planning includes prompts to guide you in creating these letters.
Financial Organization
Financial organization can feel daunting, but ensuring that your beneficiaries are current and match any wishes spelled out in other documents is a great place to start. Just In Case Planning also includes forms to list your financial accounts and creates a downloadable document where you have the option to fill in any online login information to securely store in the event that someone would need to access or cancel any accounts.
Digital and Physical Clean Up
In this digital age, almost all of us have bills we pay online, automatically, that we may not even think about from month to month. Just In Case Planning provides a form for you to list out all recurring charges (things like streaming services, cloud storage, subscription boxes, etc.) that hit your account every month/quarter/year that would need to be canceled or transferred in the event of your death.
Physical clean up should not be overlooked either. Does someone else have a copy of your house key? Does someone else know your home security code? Does someone else know where your storage unit is? Are there items in your home that a loved one might find upsetting? These are details that are often overlooked when planning for “just in case.”
Just In Case Planning
The free resource, Just In Case Planning helps people work through the process of preparing for the inevitable by keeping track of pertinent end of life documents, recording funeral considerations, creating a digital clean-up plan, and providing a space for reflections and messages for loved ones.
Peace of Mind
The Just In Case Planning tool is a wonderful gift to leave for those who want to honor your wishes and may not know your preferences. You have the ability to update and modify your preferences, and the information is available to those individuals to whom you have granted access. One never knows when an accident or illness may impact our ability to function. There is now a place where your “critical” information about your preferences and wishes can be readily available to those that need to make important decisions on your behalf. Give the gift of peace of mind not just to yourself, but also to those who are important to you.

Caregiver Stress: It’s Not What You Think

Introduction
A quick Internet search for “caregiver stress” will yield millions of results. Everyone has an opinion on the topic, and there are more statistics than you can imagine. There is even a diagnosis called “Caregiver Stress Syndrome.” This is obviously something very real, impacting the caregiving community. So how do you treat the problem? Again, back to your Internet search and you will find oodles of symptom management pages, but in my opinion, there lies the real problem. People are treating the symptoms.
Treating Symptoms V. Cause
Let’s look at how the Mayo Clinic suggest treating caregiver stress. I’m selecting the Mayo Clinic because they have published a position paper and they are a recognized authority in the medical community. To summarize the article’s strategies for dealing with caregiver stress into one sentence, it states: accept help, focus on what you are able to provide, set realistic goals, get connected, join a support group, seek social support, set personal health goals, see your doctor.
I’m going to suggest to you that these strategies address the symptoms of caregiver stress, not the cause. If the goal is to minimize caregiver stress, then the focus has to be on addressing the cause, not the symptom.
Stress Identification
To address the cause of caregiver stress, proper identification of stress is needed. The Merriam-Webster dictionary definition of stress is “a state of mental or emotional strain or tension resulting from adverse or very demanding circumstances”. The Cleveland Clinic defines stress as “Stress is the body’s reaction to any change that requires an adjustment or response. The body reacts to these changes with physical, mental, and emotional responses. Stress is a normal part of life. You can experience stress from your environment, your body, and your thoughts. Even positive life changes such as a promotion, a mortgage, or the birth of a child produce stress.” I believe the Cleveland Clinic is getting closer to the root cause, but feel they come up short on providing the caregiver with the tools to address stress.
The Definition
Enough of dodging the topic! So, what is my definition of stress? Stress is the misalignment/mismatch of expectations. It can occur in your job or personal life. It may manifest from:
- Poor communications
- Urgency pressures
- Surprises
What Can You Control?
As a caregiver, you must recognize that you can only control what is within your control. For everything else, consider:
- Make recommendations to counter what is outside your control
- Delegate or ask for specific help
- Clarify communication
- Escalate to the next level of management
- As a last resort, remove yourself from the situation (temporarily or permanently)
Take a moment and digest this definition … stress is the misalignment/mismatch of expectations. The traditional approaches to addressing stress focus on caregiver self-care, such as taking a walk, listening to music, journaling, meditation, etc. These approaches are important but do not address the mismatch of expectations that is causing the stress. Now, let’s apply it to some caregiver situations and see how you might reduce your stress by setting and managing expectations.
Application
| Situation | Action |
|---|---|
| Stressor: Insufficient supplies provided by agency. For example, you expected 1 week of medication/supplies and received a partial shipment. Mismatch of Expectations: Due to a limited amount of supplies, causes stress to the caregiver. Now they have to scramble and obtain necessary supplies. | 1. Contact agency nurse / representative 2. Review care plan with agency; learn why the supplies were cut 3. Address with the agency the necessity for the supplies 4. Obtain agency commitment to provide the ordered supplies and that care is not interrupted 5. Escalate as appropriate with agency and/or physician |
| Stressor: Home health aide does not arrive for the morning shift, as scheduled, and did not advise anyone. The patient is alone with limited mobility and needs assistance with activities of daily living. Mismatch of Expectations: Due to poor communication or scheduling, the patient is in a compromising situation and needs immediate assistance. Someone must arrange for a caregiver and provide the caregiving services until a caregiver arrives. | 1. Contact agency nurse / representative 2. Find someone to provide immediate caregiving services 3. Address with staffing problem with the agency 4. Develop a backup caregiving plan |
| Stressor: Loved one is declining faster than expected Mismatch of Expectations: The stress from this situation can impact your loved one, family, and the caregiver. Common reasons may include: a lack of understanding of the condition progression, an unwillingness to accept the diagnosis, or unanticipated complications. | 1. Write down questions to ask the healthcare provider 2. Obtain an understanding of the current symptoms are temporary or a decline in condition 3. Determine if clinical information is being kept from the loved one, causing them distress 4. Seek clarification on the care plan |
| Stressor: Ineffective handoff between caregivers causing care or treatment to not meet the loved one’s needs Mismatch of Expectations: The stress from this situation can impact your loved one, family, and the caregiver. Common reasons may include: poor communications, lack of follow-through, or comprehensive documentation of care. | 1. Define how you will communicate. This can be paper, whiteboard, app, etc. 2. Define the items that must be discussed and documented at each handoff. E.g. medications, vitals, feeding, toileting, pain & symptom management, level of consciousness and mood |
It is my sincere hope that I have offered you a different perspective on how to better understand and manage caregiver stress.
How Can Caregivers Protect Themselves and Remain Safe?
Introduction
My name is Rachel Blackwood, PT, CAPS with Designing Independence, and I’d like to address the physical burden of being a caregiver. Being a caregiver is no easy task, and caregiver safety is an important one to discuss.
We all know that self-care is important – whether you are a caregiver or not. Find time to exercise, even if it’s just a walk around your neighborhood. Allow friends, families and health care professionals to assist you – you will need their help. Finding a network of support is essential to your health, and to the health of your loved one.
Caregiver Safety
I’d like to focus on your safety as a caregiver. Your personal safety is SO important, particularly if you are the primary caregiver. If you are incapacitated from an injury, who cares for your loved one? While no one can eliminate the risk of injury entirely, you absolutely can reduce your risk of injury by taking the proper precautions.
Body Mechanics
The first and most important aspect to consider is your body mechanics. Keeping proper body mechanics is difficult when assisting another person, but it is essential for their safety as well as your own.

Lifting
Keeping your spine straight and bending your knees so you can lift with your legs is imperative, whether you are helping someone go from sitting to standing or lifting groceries. Stay as close to the person as possible when offering physical assistance.
Wheelchair Transfer
If your loved one is in a wheelchair, make sure the wheelchair is as close to the surface you are transferring to as possible. Removing leg and armrests can reduce the number of obstacles you have to manage while getting from point A to point B. Also, make sure the chair is locked.
Be sure to have your loved one scoot closer to the edge of the chair/wheelchair and make sure their feet are underneath them. Some people find a gait belt or transfer belt to be useful when assisting another person.
Communication
Communication with your loved one is critically important but can be challenging if cognitive issues are present. Sometimes those with dementia can understand what you are saying, but it takes them longer to process the instructions. Simple, one-step instructions keep the task from being overwhelming.
What are some common mistakes?
As a physical therapist, one very common mistake I see is not allowing someone to do as much of the movement as they possibly can. When assisting someone from point A to point B, very little physical lifting should be done by the caregiver. In talking with families, I’ve discovered some reasons why this might occur:
- The caregiver is in a hurry
- I can understand this, we all have schedules to maintain and keep. But even just another couple of minutes (maybe even seconds) can ensure the transfer go smoothly and without injury for either party
- The caregiver is fearful
- Often the caregiver is so fearful of their loved one falling and injuring themselves, that they complete most of the work of the transfer. Unfortunately, that puts both parties at risk.
- The caregiver lacks proper training
- In order to maximize safety for your particular situation, it’s best to have a physical or occupational therapist do a family training session where proper lifting techniques are covered. The therapist can also help to troubleshoot the unique challenges to your situation.
- The caregiver doesn’t want to see their loved one in pain
- No one wants to see a family member suffer from the pain of an injury or illness. But in most instances, your loved one will have less pain by completing the task as independently as they can.
- The caregiver thinks their loved one lacks strength
- In my experience, most caregivers underestimate the physical strength and ability of their loved ones. You can be close by and ready to offer assistance, but let your loved one try to complete the task independently. When your loved one can complete the task independently, it safeguards you from injury. It also allows them to keep some dignity and pride from being able to complete the task.
Lift Equipment
If your loved one truly is too weak to complete the task, then lift equipment may be needed. A physical or occupational therapist can help you determine if and what kind of lift equipment would be beneficial.
Hospital staff members go through regular training on how to use lift equipment, like a Hoyer lift. Caregivers will need the same kind of training to ensure their safety and the safety of their loved ones.

Caring for a loved one is a daunting task, but seeking out the training and the safety you need can protect everyone from injury. The expertise of health care professionals can give you the confidence and information you need to best care for your loved one.
Guest Blog Post
Thanks to Rachel Blackwood, PT, CAPS with Designing Independence for sharing important information on caregiver safety. Maintaining proper body mechanics is vital for the caregiver. Should the caregiver, unfortunately, suffer a back injury that complicates the caregiving routine and may present additional hardships.

Your 2019 Year End Personal Report Card
As 2019 draws to an end, this is a time to conduct your personal end-of-year review. It is time to go beyond reviewing your financial health. Check the status of investments, legal documents, retirement contributions, and making last-minute donations to charitable organizations. Take advantage of funds left in your Flexible Spending Account (FSA) and get needed dental work, glasses, or other medical services that have been delayed. Don’t stop there; financial paperwork is only a piece of your year-end personal report card.
Financial health, physical assessments, and medical treatments are not the only areas in need of attention. A key area is a review of your Advance Directive paperwork. Who knows your wishes and will speak for you when you are unable to speak for your self? Advance Directives are crucial for individuals of all ages, as serious accidents or illnesses are unexpected.
Consider:
- Do you have an Advance Directive?
- Does your Living Will reflect your current wishes?
- Have you had a health crisis since outlining your wishes and your forms need modifications?
- Are your choices of Healthcare Surrogate and Financial Power of Attorney still appropriate?
- Are those individuals still able to carry out your wishes?
- Are any home modifications needed to remain safe, and age in place?
- Do you need to purchase Long Term Care Insurance?
- Do you need to self-fund for long term care needs?
- Is your Last Will & Testament up to date and reflect your current wishes?
- Do you need to update beneficiary information?
- Do I want to be an organ donor?
On the relationship side, what needs repairing or recharging?
- With whom do you need to offer an apology or make amends?
- Who do you need to honor, recognize, or thank for acts of assistance or kindness?
- Do you want to reconnect with someone you have missed?
- What do you want to complete, accomplish, or address in the new year?

Remember
Don’t forget about yourself! Address outstanding issues, declutter material and outstanding relationship stress. Be sure to do something special for yourself each day. Make the most of the time allotted. Share your gratitude with someone who could use a kind word, smile, or a hug.
Resources
Resources for Advance Directives include: The Five Wishes, Death Over Dinner, and The Conversation Project. The holidays are a great time to share your wishes with family, allay their concerns and address any questions that surface. Having your family around to hear from you directly what your end-of-life wishes are, and how you want to be cared for when you are unable to share your care wishes, is a gift. It is often a very hard gift to share, due to the emotions associated with recognizing that you are sharing how you want to live while dying. Once shared, you will experience peace of mind and know if there are any issues between family members that need to be resolved.
Check out Home Hospice Navigation: The Caregiver’s Guide for additional information. Free resources and links available at www.JudithSands.com
Count Your Blessings
“Always keep your head up, because if it’s down you won’t be able to see the blessings that have been placed in your life.” – Anonymous

Thanksgiving is a time of reflection and introspection. How often do you stop and acknowledge the blessings in your life? As an individual with a chronic, or life-limiting illness, or a caregiver who is constantly in the caregiving mode, life can often feel bleak. It is so easy to focus on the decline in health and mentation, loss of function and of independence.
The increasing tasks of providing care occupy more and more time. They may be increasing in frequency and complexity. All this means that one is paying less attention to the activities and things that brought us happiness and peace and being more attentive to the various losses.
There are a few things that are easy to do and can help you be more attentive to those not so obvious blessings.
- Keep a journal of all the positive and happy moments. Capture the warm greetings that were shared with you by a special friend, note something funny your loved one said, write about how you felt when a meal was dropped off to you or someone did something helpful for you, memorialize something special that you saw out the window
- Play favorite pieces of music or songs that were special to you and your loved one, note the response
- Cherish the acts of “goodness” and kindness, expressed towards us, they are humbling. Acts of kindness alert and force us to acknowledge that we have “forgotten” to appreciate the goodness around us
- Reflect on all that is beautiful, good, and kind around you
- Reach out to someone; pay it forward! Return kindness and acknowledge those special individuals for what they do for you
May this Thanksgiving be a time of blessings for you and your loved ones.

Resources:
Home Hospice Navigation: The Caregiver’s Guide
Judith R. Sands
Birthrights & Deathrights, a 21st Century View

The concept of “Birthrights,” the privilege of inheritance, or right of possession, is a biblical honor traditionally associated with the first born son. Over time, the rules and customs associated with inheritance, have changed and become broader. Birthrights have caused heartache to many a parent and child.
I challenge you to think about the patriarch Isaac, the humble one, the patriarch we know the least about. Looking at Isaac from a 21st-century perspective:
- Isaac is the very late in life child, whose father tried to sacrifice him.
- He suffers from post-traumatic stress and had major trust issues
- His half-brother was sent away
- He had only one wife
- Did not get a second Hebrew name
- Never got to travel outside the land of Israel
- Had twin children with acute sibling rivalry that is still raging today
Isaac is described traditionally as having no great faults, no striking virtues, and also described as the “Master of Suffering.”
I am asking you to come with me on an uncomfortable and unusual journey. I want to focus on Isaac’s last phase of life, the time frame leading up to the deathbed. Typically, when I reference end-of-life or death, it is a conversation stopper. Indulge me. Deathrights. Yes, the concept may seem rather prickly, unfamiliar, and strange. This part of the story is not vividly described, and I want to offer a 21st century and somewhat clinical perspective to this endlessly rich and very relevant story.
Abraham was the father of pre-need planning, he wanted to be sure there would be no issues with Sarah’s final resting place. So he purchased the Machpelah in Hebron and established the family plot. This was a GIFT, one less detail for Isaac’s family to contend with, at the time of his death.
Details of Isaac’s later years are sketchy, his weak eyes, a metaphor for his inability to see what his twin sons, Jacob and Esau, needed from him. The dramatic events associated with, and leading up to his deathbed vigil, need further exploration.
It is doubtful that Isaac had an Advance Directive, the set of documents that he would have completed articulating and recording, how he wanted to be cared for during the last phase of his life. Isaac did not have access to the life-prolonging medications, technology, and treatment options that are available today.
Isaac probably wanted to be kept comfortable, have his symptoms controlled, be pain free, with loved ones around; without having to deal with family conflicts or unresolved business issues.
Maybe he had Palliative Care services for symptom management prior to his Home Hospice care. 75% of Americans want to die at home, yet only 25% actually get that preference honored.
The Living Will outlines the interventions wanted and not wanted during the last phase of life. Unfortunately, that can come at any age; these documents become effective when we are unable to speak for ourselves.
Who was the healthcare Power of Attorney or surrogate; the individual Isaac designated to speak on his behalf, when he was unable to express his wishes?
- Was it Esau, as the oldest son in this patriarchal society, prior to his birthright being diverted?
- Was it Jacob?
- Was it Rebecca as the wife? Did she have Isaac’s Advance Directive knowledge?
- Did Isaac and Rebecca have that crucial conversation, and share with each other how they wanted to be cared for if they could not articulate their wishes?
- Who had the authority and responsibility, for both healthcare & financial decision making?
- Most states, not all, acknowledge that the spouse has the legal authority to make these decisions.
Isaac had a Circle of Care, the group of individuals who came together to care and support him.
- For Isaac, it was a dysfunctional family, plagued by feuding, deceptive children with unresolved conflicts. His family, like many throughout the generations, contended with favoritism, conflict, and lack of trust.
- These dynamics impacted the communication and interactions with the loved one.
Hopefully, Isaac took advantage of the Medicare Annual Wellness visit and discussed Advance Care Planning with his physician. This preventative health service is without a deductible or co-pay. What a way to save a few bucks! Eliminating cost as a barrier, to this very important conversation.
Hopefully, Isaac got all the benefits of Comfort Care; that is Hospice Care, to alleviate and manage his symptoms of restlessness, agitation, pain, shortness of breath, or other signs of discomfort. No doubt his Palliative Care or home hospice team worked closely with the family to support and comfort them, as they addressed Isaac’s needs.
- It is hard to say whether Isaac was the victim of health care fraud. With all probability, his Medicare or insurance cards were not used inappropriately. Yet the fraud highlighted in the Torah relates to the birthright is well known.
Why am I proving a 21st Century perspective on this Isaac? November is National Hospice and Palliative Care Month. Professionally, I worked with many families having to make end-of-life decisions. Unfortunately, there were too many times where loved ones did not verbalize or document their wishes. This places an undue burden on family members and care partners. This can result in unnecessary conflict between family members who may have competing perspectives and wishes for end-of-life decision making.
The Advance Directive needs to be communicated so that those loved ones left behind should not have to make unnecessary decisions. As mom went through her home hospice journey, she often said: “What do families do without someone with your knowledge and experience?”
There are a number of resources to assist you while coming to terms and thinking about end-of-life wishes. One of my favorites is the Conversation Project from the Institute for Healthcare Improvement (IHI) which is dedicated to helping people talk about their wishes for end-of-life care, for both adults and children. The Conversation Project provides clear information about available options, in many languages.
Another wonderful resource is Death Over Dinner. It can be utilized by a group of individuals who come together over a meal, to explore end-of-life wishes. A family may dedicate the Thanksgiving meal as a time for the senior generation to share their end-of-life wishes and provide a safe space for discussion and clarification. I am happy to help you secure these helpful resources.
Honoring your child, discuss your preferences with your children, share how you want to live during your final days.
- This is especially important if there are estrangements. Unresolved family issues too often resurface at a time of crisis and your wishes may not be honored, if the wishes are not clearly known to all involved.
- For those who are not in traditional relationships, share these wishes and expectations with a friend or partner, I call this honoring a friend. Hopefully, this is a mutual process where you can advocate for each other.
- Having Advance Directive paperwork formalizes the process.
- Advance Directives should be updated and modified over time.
The final phase of life can be a time for blessings, a time to address unresolved family issues, a time to be mindful and appreciate what life still has to offer. A time to put closure on your affairs, the way you want, alleviating that responsibility from others.
Something all of us should and can do, is support a caregiver. Caregiving is challenging, it is an ever-changing demanding role.
- Caregiving typically becomes more demanding and complex as a loved one declines.
- Specific acts of kindness – such as a meal, a ride or running an errand, make the caregiving routine so much easier.
Know your wishes, share them, and unburden your loved ones.
Resources
November 2019 is Palliative and Hospice Care Month

Annually in November, Palliative & Hospice Care services are recognized for the vital work done for those in need of symptom management and comfort care. Appreciation and recognition of the unique professionals dedicated to controlling symptoms and providing end-of-life care helps spread awareness. November is a perfect time for individuals of all ages to discuss their end-of-life preferences and wishes, with loved ones and physicians. Take the time to formalize, complete, or update Advance Directive forms, since your wishes may have changed. Do not forget that those previously identified to take on the management of your care and affairs, may no longer be available or capable of assuming the role. New healthcare surrogate and financial power of attorney may need to be named. Consider sharing your preferences and wishes at Thanksgiving with family and friends, providing the opportunity to share your desires and address expressed concerns or anxieties.
Advance Directive Consideration
There are many resources available to help you get started in identifying and expressing your wishes. In reality, for most people, it is not something that can be done over coffee. A bit of soul searching and reflection on how you viewed the experiences of friends and family that have gone through the dying process. Think about what you thought went well, and what made you uncomfortable. How you formulate your individual Advance Directive will be shaped by many aspects including your culture, values, experiences, religion, relationships, and environment.
Advance Directive Resources
- Conversation Starter Kit a resource that is available in multiple languages includes a version for those with Alzheimer’s/dementia and those with a seriously ill child. These resources are from the Institute for Healthcare Improvement (IHI).
- Death Over Dinner that helps you plan a dinner party to articulate end-of-life preferences. “The dinner table is the most forgiving place for difficult conversation. The ritual of breaking bread creates warmth and connection, and puts us in touch with our humanity.” The site has a number of versions including an Australian, Jewish and Brazilian edition.
- Five Wishes is a complete approach to discussing and documenting your care and comfort choices. It’s about connecting families, communicating with healthcare providers, and showing your community what it means to care for one another.
- Cake an interactive end-of-life planning website that helps people plan ahead for healthcare, legal, funeral, and legacy decisions. A checklist guides users to create and/or upload important documents (like POLST) that express their final wishes. Users can share secure access to their end-of-life plan with anyone who has an email address. Cake’s mission is to empower everyone to receive end-of-life care that aligns with their values and wishes.
Aging in Place
As you address your Advance Care Planning wishes, remember that aging in place may be part of your plan.
- Consider is your current home going to meet your needs or will modifications be necessary?
- Can the expressed wishes be honored in your current home environment?
- Will you in need of home modification as your condition or your loved one’s condition changes?
- If there are anticipated condition changes, what will need to happen so that you or your loved one can remain at home?
- Have you taken the measures to reduce clutter and minimize trip and fall hazards?
The American Occupational Therapy Association has many resources to help you find the appropriate entity to assist you aging safely at home. In Raleigh, NC consider the services of Designing Independence, they bring clinical expertise to focus on your particular aging in place needs.
Resource
Medication Overload, Polypharmacy and Me
A critical issue for older adults is the hidden drug problem of medication overload, also known as polypharmacy. This refers to when individuals use multiple medications and the harm, or potential harm of taking the medications outweighs the benefits. Harm increases with the number of medications taken. “Getting medications right is essential because when your medication is wrong, your mental activity can be off, your mobility can be compromised, and what matters to you will not be front and center.[i]”
What is Polypharmacy?
Polypharmacy is typically defined as taking five or more medications at the same time. Over 40% of seniors are taking five or more prescriptions daily. 20% of seniors take ten or more medications and those with multiple medical conditions may be taking even more than that.
Why is Polypharmacy a concern?
As individuals age, there is a decline or weakening in organ function over time. This means that older individuals, especially those with acute or chronic conditions do not process the medication as quickly, as well, or readily. This places the individual at greater risk of side effects. Cognitive impairment and osteoporosis are two common serious side effects of polypharmacy. When these individuals fall they are more likely to suffer a hip fracture than younger individuals[ii].
“Medication overload will contribute to the premature deaths of 150,000 older Americans over the next decade and reduce the quality of life for millions more.[iii]”
How Can I Lower my Risk of Polypharmacy?
- Keep a complete written record of all medications taken, that includes supplements, vitamins and any over-the-counter medications
- Review the at each provider visit, be sure to ask if you really need to be taking all the medications, ask if there are drug interactions between any of the medications that you are taking
- Fill prescriptions at one pharmacy so that you can your pharmacist has a complete record of all the medications and can intercede with providers if any prescription red flags surface. Be sure to share all the supplements, vitamins and any over-the-counter medications
- Participate in “Brown Bag” medication sessions where you take all of your medications and your supplements, vitamins and any over-the-counter medications and sit with a pharmacist to have a review of what you are taking for side effects and over medication
Polypharmacy is Under Recognized
Medication overload or polypharmacy is the drug problem that is not getting headlines; it is a serious and growing issue impacting the aging populous. Protect yourself and be proactive in minimizing your risks. This problem cannot be ignored as implications to you are high.
Reference:
[i] The Hidden Drug Problem of Older Adults: Medication Overload
[ii] Medication Overload: How the drive to prescribe is harming older Americans
[iii] Solving Medication Overload: America’s Other Drug Problem

Helping Someone Grieving– What Should I Do?
When someone you care about suffers a loss, they need continuing support. Immediately after the loss there are frequently many people around providing food and comfort. Since the loss is fresh in the minds of supporters, they tend to bring the meals of comfort, send texts, notes, and flowers, help with chores, and other gestures of support. This support tends to wane as the time goes on, leaving the mourner at times alone.
Grief is an individual process with its own unique timeline. How an individual grieves for one loss does not predict how they will grieve for a different loved one. As one journeys through Dr. Elizabeth Kubler-Ross’ Five Stages of Grief (denial, anger, bargaining, depression, and acceptance), they are not linear stops, and the grieving person may go backward and forward through the stages several times. The relationship between the individual grieving, the loved one, and the circumstances of death often impact the grief journey.
Considerations
What was the relationship between the individual mourning and the loved one? Were they happy or estranged? Did they communicate frequently or was there a lot of “unfinished-business” between them? Consider if the death was anticipated and came after a long illness or was the result of a tragic accident. Had the loved one been taken at a young age with a bright future ahead, or had the individual lived a rich and full life?
What other stressors is the grieving individual managing?
- Loss of a different family member or friend in the recent past
- Divorce or loss of a job
- Recent receipt of a terminal diagnosis or other crushing news
- Religious or cultural customs that may not be in alignment for the one grieving and other family members, making this a challenging time
Grieving is a special time for the one who sustained the loss. It is about supporting them, and not sharing our experiences with loss or reframing their thoughts. It is a time to acknowledge the loss and not ask details about the death. Respect privacy and provide a shoulder of support.
Take Action
- Keep it about the one grieving and the loved one
- Check-in regularly during the first few weeks
- Be there to listen and hold a hand, listen, sometimes silence is best
- Reach out at 3, 6, 9 & 12 months, make a call or send a card
- Acknowledge and reach out at holidays
- Pay tribute – make a donation in their memory, support a favorite cause or charity
- Don’t ignore the existence of the loved one. Mention their name
- Reach out on special dates – birthdays & anniversaries
- Avoid judging, remember that grief is individual with its own timeline

Resources
21 Ways to Help Someone You Love Through Grief

Destress – Stress Management Apps
Caregivers suffer a multitude of emotions and constantly deal with stress. Emotions may include anxiety, sadness, depression, hopelessness, and despair. Stress and anxiety, result in loss of sleep, compounding muscle tension, and a negative state of mind. Caregivers are often faced with 24/7 responsibilities. Many caregivers report that they are constantly juggling and dealing with family members who are not fully supporting them. Self-care is critical for continued well-being, staying balanced, and being able to continue caregiving responsibilities.
Many caregivers do not have the time, energy, or resources to take advantage of professional counseling. So what can a caregiver do to decrease stress with limited time, energy and funds? There are a number of stress management apps that can help individuals better manage some of the anxiety in their lives. There are apps for general stress relief, meditation, sleep, and others that support general health and wellbeing. Some of the apps are free; others have a modest fee or an associated in-app purchase.
Apps
Breathe2relax – Stress management tool, provides detailed information on the effects of stress on the body, instructions and practice exercises to help users learn the stress management skill called diaphragmatic breathing. Developed by The National Center for Telehealth and Technology, originally targeted to military veterans. Free.
Calm – Focuses on helping you calm the senses; doubles as a sleep aide since one of its features is comprised of soothing adult bedtime stories. Free trial and a subscription.
Headspace – General guided mediation is free; access to more specific meditation involves a subscription.
Stop, Breathe & Think – Check in with your emotions, mindful breathing, and meditation exercises. There is a version for educators working with students of all ages. Free trial and a subscription.
It is important to remember that apps are not a substitute for seeking professional mental health care.
Consider your stress management needs and goals; try several apps until you identify the app that will augment your self-care practices, and help you focus on managing your stress.
Resources:
Stress Relief Apps That Can Transform Your Life
7 Self-Care Apps To Help You Stay Balanced In 2019
The Best Self-Care Apps To Try If You’re Looking For Something Simpler Than Face Masks

Palliative Care – A Top Priority
The need to make quality palliative care services available across the United States is growing. The number of Americans living with serious illnesses increases annually. Palliative care is expert medical care for individuals with critical illnesses focusing on addressing symptom and stress management of a serious illness. Palliative care services are offered concurrently with other medical treatments. The goal of palliative care is improving the quality of life for patients and family members. One does not have to be enrolled in hospice to take advantage of palliative care services.
- There are over 12 Million adults & 400,000 children living with serious illnesses
- 72% of hospitals with greater than 50 beds have palliative care programs
- 66% reduction in symptom distress is reported by palliative care patients
- $3.5 Billion per year savings is possible with nationwide implementation of palliative care programs
Meeting the Need
Hospitals and physician practices are moving towards value-based reimbursement. They are expanding and redesigning palliative care programs. A key component of this process involves improving access to these symptom management services. Healthcare providers are recognizing that palliative care programs are essential to a patient’s wellbeing. They are encouraged to offer palliative care services more aggressively to better meet patient symptom management needs.
Who Benefits?
Individuals with advanced chronic conditions including heart failure, COPD, dementia, cancer patients most frequently benefit from these services. One should always ask if their particular situation would benefit from palliative care services.
Symptom Management
Common symptoms addressed by the palliative care service include shortness of breath, pain management, nausea, vomiting, fatigue, anorexia, depression, and anxiety. Symptom management approaches are customized to meet the patient’s individual needs and modified as the condition changes. The goal is to keep the individual as comfortable as possible.
Where is Palliative Care Provided?
Palliative care services anywhere ever the patient is; in the hospital, skilled nursing facility, nursing home, assisted living or home.
How to Get Palliative Care Services?
Speak to your healthcare provider to determine if you or your loved one’s clinical condition would benefit from palliative care services. Your provider will advise you of locally available palliative care options. Access to palliative care services may be limited by your geographical location, choice of providers may be restricted by your insurance provider. Should you encounter any difficulties, speak to your insurance company’s customer service department to identify a provider.
Resources
Home Hospice Navigation: The Caregiver’s Guide
Reference
https://www.aha.org/center/performance-improvement/palliative-care

Speak UpTM to Prevent Falls
The Joint Commission’s (TJC) award-winning Speak Up™ program has a new initiative focusing on fall prevention. Falls happen at home, out and about, in nursing homes and hospitals. Falls happen for a variety of reasons including loss of balance, tripping or slipping. More than one in four adults over 65 years of age falls annually. Falling once doubles the chance of a repeated fall[i]. The Centers for Disease Control and Prevention (CDC) anticipates seven deaths each hour from falls by the year 2030[ii]. The average cost of a fall with injury is estimated at $14,000. That does not take into account the impact on the individual and the fact that unfortunately, not all recoveries are complete. Falls are a real life-changing issue impacting a growing percentage of the population. There are actions that can be taken to decrease the risk of falls and injury.
Risks
The senior population is growing and these individuals want to maintain their independence. Women have a 50% greater fall risk than men[iii]. Having an alcoholic drink a week or taking five or more medications and also managing diabetes or osteoporosis increases the risk of falls[iv]. Other medical conditions contributing to an increased fall rate for seniors include angina, stroke, asthma, COPD, chronic kidney disease, arthritis, depression, and dementia[v].
Take Action
If you or your loved one has had a fall (with or without injury), contact your provider to discuss and determine if any clinical intervention is needed. Do not ignore a fall, it could be a warning sign! Get checked out before a serious life-changing injury happens.
Remove trip and slip hazards, check your footwear, have your vision checked, address any necessary home modifications needs and explore if an automatic fall response system may be appropriate for you or your loved one.
The Joint Commission has a new patient safety campaign Speak UpTM to Prevent Falls that provides information to patients and their families/caregivers on how to prevent falls and become more active in their health care. Check out the video and determine what steps and precautions you need to take to reduce the chance of falling.
Hand-out on a variety of actions to take To Prevent Falls. Print and use as a checklist. Share with a friend. https://www.jointcommission.org/topics/speak_up_to_prevent_falls.aspx
Resource
Home Hospice Navigation: The Caregiver’s Guide
References
[i] Stevens, J. A., Balesteros, M. F., Rudd, R. A., DeCaro, E., & Adler, G. (2012). Gender differences in seeking care for falls in the aged Medicare population. Am J Prev Med.,43, 59-62.
[i]Centers for Disease Control and Prevention (CDC). Important facts about falls. (n.d.). Retrieved August 8, 2019, from https://www.cdc.gov/homeandrecreationalsafety/falls/adultfalls.html
[iii] Centers for Disease Control and Prevention (CDC). Important facts about falls. (n.d.). Retrieved August 8, 2019, from https://www.cdc.gov/homeandrecreationalsafety/falls/adultfalls.html
[iv] Harvard Health Publishing. (2015, April 15). Why do women fall? Retrieved August 8, 2019, from https://www.health.harvard.edu/womens-health/why-do-women-fall
[v] Paliwal, Y., Slattum, P. W., & Ratliff, S. M. (2017, March 28). Chronic Health Conditions as a Risk Factor for Falls among the Community-Dwelling US Older Adults: A Zero-Inflated Regression Modeling Approach. Retrieved August 8, 2019, from https://www.ncbi.nlm.nih.gov/pubmed/28459060
Speak UpTM About Your Care
The Joint Commission’s (TJC) award-winning Speak Up™ program, launched in 2002 has been used in more than 70 countries. It encourages patients and family members to speak up and be advocates for their healthcare. It is an important element of keeping patients patient safe by encouraging active participation in healthcare services. Important information that is appropriate to use in all interactions with members of the healthcare team.
- Speak up
- Pay attention
- Educate yourself
- Advocates (family members and friends) can help
- Know about your new medicine
- Use a quality health care organization
- Participate in all decisions about your care
These elements are reminders about how to be an active participant in your own healthcare and an advocate for your loved one’s healthcare services. They are practical and based on science. Try them out on your next interaction with a member of the healthcare team.
The short video is a useful step-by-step example and a reminder of how to use SPEAK Up™.
Resource
What Was The Most Helpful Surprise?

Surprise
The Cambridge English Dictionary defines a surprise as “an unexpected event, or the feeling caused by something unexpected happening.” Often the experiences of caregivers more closely match the Merriam-Webster definition of a surprise, “an attack made without warning.” As a caregiver, too often the focus is on the unanticipated crisis or the unexpected decline of our loved one. At times, the attack without warning is the daily caregiving ritual.
Caregiving Toll
The caregiver is the project manager! The individual who has taken on the role of keeping the home going, tending to the loved ones physical and emotional needs, managing medications, treatments and supplies, paying the bills, doing the wash, and all the other unglamorous activities that must get done. The stress a caregiver endures while caregiving for a loved one has long term physical effects. As family and friends of caregivers, there are specific things that you can do to bring an unexpected smile, and relieve some of the caregiving stress.
The “Polite” Offer
Too often caregivers are asked: “What can I do to help?” Sometimes it is a genuine offer and other times it is perfunctory one; similar to “Let’s get together for lunch.” The lunch meeting never actually takes place since it was a “nice and hollow” gesture. Caregivers have too many decisions to make and it is not always easy to stop and run through the “wish list” and come up with an item that matches what the requestor likes or is able to do.
Genuine Assistance
Seasoned caregivers may have a task or laundry list for just such questions, it may resemble: Please help with the following:
- Pick up the following from the supermarket
- Take out the trash cans on garbage day
- Mow the lawn
- Take the car for an oil change
- Fold a load of wash
- Make a meatloaf (or another much-desired entrée)
- Sit with my loved one while I go to the hairdresser
The Unexpected Surprise
I often ask caregivers what was an unexpected and welcomed surprise that made a difference for them. The overwhelming majority of responses related to not being “forgotten” by friends and family. Despite not being able to physically participate in their usual social activities, knowing that someone genuinely cares about them, and took the time to express their thoughts made the difference. Some caregiver responses included: getting a greeting card regularly, finding a meal or flowers at their doorstep. The fact that someone went out of their way to do that “act of assistance” without being asked made the difference.
Caregivers, please share “What was the most helpful surprise” that someone did for you. Friends and family of caregivers, take note and see how you can give a caregiver a wonderful and much-needed surprise.
Resource
What Made Me Smile Today?

Opportunities to smile while caregiving tend to be few and far between! Often, we focus most on what is not going well! The decline in our loved one’s status is easy to see. We can quickly list the things that our special person can no longer perform or enjoy. The effects of chronic illness and the decline in status are heartbreaking. Your loved one may experience: not being able to walk, losing bowel and /or bladder control, unable to recognize family members and friends, forgetting important information, no longer enjoys activities, and the list goes on.
Smiling
Changing the focus for the caregiver is not easy; it is a bit like “Is the glass half full or half empty?” Should the caregiver focus on all the challenges and decline in their loved one’s status or focus on moments of joy and levity? Caregiver “survival” is critical if that special person is going to survive, and then thrive, after the caregiving role has been completed. Smiling is a basic cross-functional form of expression a way to connect when words cannot. The act of smiling has health benefits! Smiling improves mood, may ease anxiety and depression by releasing endorphins, lowers blood pressure, boosts the immune system and can reduce pain. People who smile impact those around them in a positive way, it’s contagious. There is a whole body of science relating to the health benefits of smiling.
How To Smile While Caregiving?
Finding a smile or two in the caregiving process is not a reflection on the loved one, rather the situation and the funny things that may be said, the unexpected joke or situationally funny remark. Unintentional antics ease the tension for both the caregiver and loved one, if they are able to appreciate the situation. For some, giving funny names to parts of the day or tasks to be performed can lighten the mood and set the stage for a bit more levity. Respecting the loved one is always the first priority. Hold on to the humorous moments they are sustaining especially when times are trying. My mom couldn’t remember the name of our local grocery store, Harris Teeter’s, so she gave it the name Teeter-Totter, which has stuck with us. It brings a smile to me and my husband whenever we say it.
Action Plan
- Smile as you wake up, greet others with a smile
- Focus on the positive
- Keep a notebook of funny things and wonderful surprises that happened while caregiving. When times are tough, go back and reflect on the happier time
- Find joy in the little things. Focus on something that went well during the day; it could have always been worse!
- Note something that you are thankful for
- Start your morning or end your day by looking at the comics
- Sign up for a “joke of the day”
- Watch a funny movie
- Connect with others, be sure to ask if they had something funny or unusual happen in their day
- Find the energy and perform a small act of kindness for someone else, it will come back in spades
- Be kind to yourself; recognize that you are doing a difficult and stressful job. Eat well, stay hydrated, have a treat now and then, do something nice for yourself, sing a funny song, take a few minutes to listen to music, read or do whatever brings you joy and smiles
Resource

Bam! – You Are Now A Healthcare Surrogate
Your loved one or friend has named you as their healthcare surrogate; the individual who will authorize medical care and treatment, and make all necessary healthcare decisions should the loved one become incapacitated due to illness. This role comes with extensive responsibilities, to ensure that you are acting in accordance with the individual’s wishes and in their best interests. You need to think not of your wishes, but what your loved one would want. If you have any reservations or concerns about performing the role, the reservations must be addressed promptly. Your loved one must have peace of mind knowing that whomever they appoint as their healthcare surrogate will act in their best interest, and do so with no reservations.
It’s Not About You
It’s not about the healthcare surrogate; it’s all about ensuring the best interests for your loved one. Always try to look at things through your loved one’s eyes. Don’t just do what you would do if you had this illness or condition. Don’t let your distress about what is happening with your loved one result in you tell the doctors to do something that you know your loved one would not want.
Think about their medical condition, and how they would want to be treated. Hopefully, you have discussed their wishes and preferences before a crisis situation surfaces, so you already know what are your loved one’s preferences.
Realize that there may be another representative appointed to address the non-healthcare and financial interests of the loved one. Critically consider if you can work collaboratively as healthcare decision maker with the other individual named to protect the financial welfare of the loved one. A disservice will be done to the loved one when the healthcare and financial surrogates cannot collaboratively ensure that the loved one’s wishes are followed.
Be Prepared For The Role
At the time of being named as a healthcare surrogate, you need to know your loved one’s medical status.
- Discussed your loved one’s wishes and have a clear understanding of their end-of-life preferences
- Have a copy of the Healthcare Surrogate form
- Named on HIPAA Privacy Notices that the loved one has completed at each of their medical providers
- Does the person have any ongoing medical issues, such as chronic conditions?
- Does the person have any allergies (to medicines or to other things)?
- Is the person currently taking any medicines or receiving any medical treatments? What medicines or treatments and for what purposes?
- Are there any drugs or medical treatments that the loved one would prefer not to receive, and why?
- Meet/get to know the financial surrogate if applicable. Exchange contact information
End-Of-Life Preferences
Many times the healthcare surrogate assumes the role to address end-of-life care. This typically happens when there is a crisis situation and quick decision making is needed. This is the time when knowing and following the loved one’s advanced directive and planning wishes takes center stage.
- Does your loved one care more about living as long as possible (even if that might mean some physical discomfort), or being as comfortable as possible (even if that might mean a shorter life)?
- Does your loved one want to be at home at the end-of-life, or would the loved one prefer to be in a hospital or professional care setting?
- Does your loved one have religious or spiritual values that will affect the types of care or treatments he or she would like to receive?
- Are there specific life-support treatments that your loved one knows he or she would like to receive or would not like to receive?
- Would your loved one like to have a palliative care team or hospice team care for him or her at the end of life?
- Are there other wishes that should be observed as your loved one nears the end-of-life, such as calling a religious leader to come visit the person, having certain music playing, or having certain friends or family members in the room?
The Job Description
Key responsibilities and duties of the healthcare surrogate (there is always something else you may have to address). There may be some modifications to the role based on State statutes; the following is a general guide:
- Make decisions that are in accordance with your loved one’s wishes including religious and moral beliefs, if those wishes are known
- Make decisions based on the patient’s best interests, if the patient’s wishes are not known
- Diligently consult with physicians and other health care providers regarding medical care, including medical tests, medicine, surgery or end-of-life care
- Provide informed consent on in matters of medical intervention
- Apply for Medicare, Medicaid, or other programs or insurance benefits on your loved one’s behalf to help pay the cost of health care
- Manage the admittance to or transfer from health care facilities, including hospitalization, rehabilitation center, nursing home, home health care or hospice
- Authorize access to your loved one’s medical records for healthcare decision making
- Authorize release medical records to third parties
- Authorize decisions regarding autopsy, organ and tissue donation
- Request or decline life-support treatments
- Choices about pain management, including authorizing or refusing certain medication or procedures
- The option to take legal action on the person’s behalf in order to advocate for his or her health care rights and wishes
Resource

Your Spokesperson – Your Champion
Who will speak for you?
Designating someone to serve as your representative to make healthcare decisions for you, if you are unable to make them yourself, is an important activity. The designation of this role is a key component of Advance Care Planning (ACP). Determining who that champion of your medical decision making should be when you are incapacitated requires some thought. Often a spouse or partner is the obvious choice. Hopefully, these individuals know your wishes and will do whatever it takes so that your wishes and interests about medical care, treatment, or no treatment will be honored. In the absence of a spouse or partner, consider naming your adult child or a trusted friend for the task. Remember, whomever you choose to serve as your healthcare surrogate/proxy, they will be an integral part of your circle-of-care.
When no one can speak for you…
In the absence of a named healthcare surrogates, healthcare power of attorney, or healthcare proxy (similarly known documents) most states have a hierarchy of who will take the responsibility for making your healthcare decisions. A guardian may be appointed by the Courts in the absence of a family member or trusted friend who knows your wishes. A guardian may also be appointed in the event that there are concerns in how the healthcare surrogate is making decisions relating to your healthcare needs. Typical situations where guardians are named include the healthcare surrogate not following your wishes or making decisions that are not in your medical best interest.
A healthcare surrogate has been identified
Once you have identified the individual who will be serving as your medical champion, verify that they are willing and able to take on this responsibility. Once you have their confirmation that they are willing to take on the role, it is necessary to complete the appropriate forms designating your wishes. Healthcare surrogate/proxy forms can be obtained free from your physician, hospital, State Agencies, or may be obtained from an attorney as part of your Advance Care Planning packet for a fee. Most states require that the forms be notarized.
What to do once the surrogate has been identified:
- Inform the individual that they have been named and get their agreement to be the surrogate
- Provide a copy of the form to the healthcare surrogate/proxy so that they can present it in an emergency to help in ensuring your wishes are respected
- Provide the healthcare surrogate/proxy’s name and the individual’s contact information to all your healthcare providers
- Add the Healthcare surrogate/proxy to Privacy Notices that you are asked to complete and acknowledge with medical providers. Without this information, they may be unable to communicate your medical condition and information on your behalf
- Keep that healthcare surrogate/proxy’s name and contact information with you in your wallet and provide with any medical reports or information
- Keep a copy of the Healthcare surrogate/proxy form readily available; do not place it in a safe or bank vault that might not be accessed in an emergency. The form must be handy in the event of a medical emergency. Some individuals keep a copy on their refrigerator, a common location that EMS will check for such documents
- Upload your healthcare surrogate/proxy document to your state’s registry (if available)
The healthcare surrogate can be changed
The designation of a healthcare surrogate/proxy may be changed. This can occur if you feel that the initially appointed individual is not able to act in your best interest, or is no longer able to fulfill the role. If that is the case, you will need to thoughtfully identify a new healthcare surrogate/proxy, complete new a new form, and diligently go through the steps with your providers to update the surrogate designation and privacy forms. The outdated contact information and forms should be removed from wallets and replaced with the new information.
A future blog post will address the role of the healthcare surrogate.
Unfinished Business

Typically when hearing the phrase “Unfinished Business”, the first thought is that of a work or household task that has not been completed. You may have been called away, distracted, or interrupted and did not have the opportunity to complete the job. Yet there is another meaning to the phrase “Unfinished Business” that goes beyond tending to the outstanding tasks (incomplete personal and work projects) and encompasses the spiritual distress associated with relationships, unresolved matters from the past, and may not be religious in nature.
As an individual’s physical status declines, they have lower energy and concentration levels, and may not be able to focus on managing their outstanding issues. This makes addressing “Unfinished Business” a priority for family and caregivers who work with those in declining health.
Approaches
An approach to addressing “Unfinished Business” is by asking your loved one:
- Is your “Unfinished Business” going to be a surprise or a burden to someone you love?
- If you had an opportunity to say something to your family member, what would it be?
- How are your spirits holding up through all of this?
- What is like to be you right now?
Your loved one may ask you for guidance and assistance with some of their concerns.
Depending on the circumstances that have led to the individual’s physical decline, there are various types of questions that people ask themselves and others, as they realize their time is limited. In many cases, there are no real answers, yet these questions drive home the point that opportunities should be provided for the loved one to put closure on their “Unfinished Business.”
Loved Ones Questions
Questions your loved one may ask that provide some insight as to concerns about their current status or legacy:
- Meaning: How do I explain this to my kids?
- Purpose: I feel so useless.
- Suffering: Why is this happening?
- Connection/Legacy: Will my kids remember me?
- Permanence: Will I live on in some way?
- Coping: How am I going to get through this?
As a family member, friend, or caregiver you need to be prepared for such questions and provide the loved one an opportunity to share their thoughts and feelings without being judged. Avoid the temptation to dismiss having this emotionally charged conversation; remember that it is not about you, it is about the loved one having the opportunity to put closure on their issues and concerns. Additional support and assistance may be obtained through clergy, hospice staff, social workers, nurses and individuals that the loved one trusts and values.
Advanced Care Planning- The Gift of Love
National Healthcare Decision Day
April 16 is National Healthcare Decision Day is an initiative to encourage individuals to express their wishes regarding healthcare. Sharing your wishes relating to end-of-life, should not take place during a crisis. Additionally, the discussion is not reserved for those in retirement.
A medical crisis could leave you unable to make your own healthcare decisions. The discussion should take place early in life. Your views relating to end-of-life care and preferences are shaped by many factors including culture, religion, ethnicity, educational level, beliefs, family customs, income, environment and exposure to those who are chronically ill or dying.
The importance of younger adults considering their end-of-life wishes cannot be understated. Younger adults have a lot at stake. If stricken by serious disease or accident, medical technology may keep them “alive” for decades. Some of the most well-known “right to die” cases resulted from young individuals, incapacitated by tragic accident or illnesses and maintained on life support.
Advance Care Planning
Advance Care Planning (ACP) is a framework to help you think about the various plan components, discuss and decide what is right for you, document and share your wishes. Then periodically review your wishes to determine if any changes need to be made. You should determine who will be your Healthcare Champion (Surrogate), the individual who respects your wishes and will speak on your behalf if you are unable to do so. Empower this person by completing a Durable Power of Attorney for Healthcare Decisions also known as a Healthcare Proxy document.
When you document your end-of-life wishes, it is vital that you share them with your surrogate and loved ones. Your surrogate should have the opportunity to seek clarification from you and not be surprised at a time of crisis by your wishes. This provides you the chance to validate that your wishes will be respected.
Advance Directive Considerations
When thinking about your Advance Directive there are several important questions to consider:
- What is important to you?
- What do you want to happen?
- What do you want not to happen?
- Who would speak for you?
Resources
There are wonderful free resources to assist you in opening the discussion with loved ones, and helping you to define your wishes. Many of these resources are also available in a number of foreign languages.
Updating and Ensuring Availability of your Advance Directive
Your Advance Directives can always be modified. It is a good practice to review your wishes every year or so, and when there is a major change in health status. Updated documents need to be shared with the Healthcare Champion (Surrogate), your physician (medical team), and uploaded to a registry if available in your state. Avoid placing such documents in a safe deposit box as they will not be accessible if the bank is closed. Consider uploading to your smartphone for back up.
The Caregiver Match
Caregiving is like dating
I often share that finding the right caregiver is like dating. There needs to be a comfortable connection between the loved one and the caregiver. The circle-of-care members (family and significant others) must also feel at ease with the hired caregiver. Getting to that point can be painful and frustrating; just know that there is a caregiver match for every loved one!
Finding the right match involves the “personality” component and a “skills” portion. However, addressing each of the caregiver components for a match is critical for a safe, respectful and lasting caregiving relationship. If there are questions or concerns relating to a caregiver, never settle; don’t make do with a hired caregiver. There must be both a personality and skills match. Above all, you always have caregiving options (caregivers may be hard to find at times). As a member of the circle of care, you must be assertive and protective of your loved one. Remember, not all caregivers are the same.
Matchmaker, matchmaker
For some loved ones, addressing the personality component may be more difficult. Consider the highly educated individual with lots of professional affiliations and hobbies who may be physically limited, yet is used to very stimulating discussion and is unable to re-channel the energy and thoughts in other ways. Can the caregiver adapt their individual style to listen and ask questions, or do they show disinterest and disregard for your loved one?
There are those caregivers that are more comfortable tending to the mechanical care aspects and prefer limited verbal communication with the loved one. On the flip side, there are those caregivers with the “warm and fuzzy” personality who can engage the loved one, however, they are not as focused on the caregiving mechanics. The challenge is finding the right balance of engagement and caregiving mechanics. Find the individual who has both a head and heart while caring for your loved one.

Red flags:
- Appearance – Uniform: was the caregiver working elsewhere (in the same uniform) prior to coming to care for your loved one? Was that individual working at a daycare center during flu season or with others who may have an illness that could be spread? Safety of the caregiver is paramount. Paid caregiving is done with closed toe shoes for the caregiver’s protection. Flip-flops or open toe shoes should raise
a concern . - Long acrylic nails – The issues of infection control and acrylic nails is well documented. Long nails and fragile skin do not mix. The risk of skin tears is real, and skin tears often come about when holding or repositioning a loved one. You want to minimize injury from nails or jewelry that could unintentionally harm your loved one.
- Correct use of equipment – Knowing how to use the medical equipment correctly seems basic, yet there are many different models of the devices and supplies used to care for a loved one (glucose monitors/pumps, pressure mattresses, CPAP, wheelchairs, mechanical and electrical beds, etc.) Is your caregiver experienced with the medical equipment, or can they receive training?
- Getting up and moving – Falls are a common cause of injury to loved ones as they decline. Often the loved one does not realize or want to recognize, their declining physical status. The caregiver needs to be proactive in responding to that change in status. Often gait belts are used as a safety precaution. If the item has been prescribed, it is imperative that the caregiver ensures its use. Concerning comments made by a caregiver about to walk a loved one that should raise concern include: “I have him” or “I can catch her” pose a risk to both the loved one and the caregiver.
- Follows instructions – It is important that the caregiver follows the plan of care. If the caregiver raises concerns or questions about the loved one’s status, those concerns need to be addressed and the care plan updated. Unfortunately, there are some caregivers who believe that they know what is always best for the loved one and disregard the professional recommendations to the contrary. Situations that should raise a concern, include giving the loved one food they may want, but are unable to tolerate or eat safely, getting the loved one out of bed or walking them when the loved one truly does not have the physical strength and ability. These types of situations place your loved one at risk.
- Receptiveness – Be aware of how the caregiver responds to simple requests and sharing of the loved one’s preferences. When resistance to care plan modifications are expressed or observed, explore the reasons further, and determine if this individual can continue as a caregiver. Be sure the caregiver feels valued and appreciated, and thanked for the activities performed. Remember that the goal is ensuring that your loved one’s needs are well taken care of. If the “I know better than you” attitude is consistently displayed, this individual may not be the right caregiver for your loved one.
- Shares updates – The majority of caregivers are very good about sharing observations and changes in the loved one’s status. That comes from building a relationship. This is a vital practice to promote and encourage. Often the caregiver will clue you into issues and concerns that a loved one may have and not be sure how to address it with you. If your caregiver is not sharing, ask for updates and let the caregiver know that you value their opinion and insights, and would like that communication.
Respecting the preferences of the loved one, and asserting for their needs is not easy. Don’t be shy. If you don’t do it, who will? Loved ones are vulnerable, their welfare and safety must be the primary goal and focus.
Finding a Caregiver is Like Dating
#palliativecare, #palliative, #hpm, #homehealth, #compassion, #eol, #caregiving
Simplifying Complex Care for Older Adults
Mary Tinetti, MD is the Chief of Geriatrics at Yale School of Medicine and Yale-New Haven Hospital, and co-chair of the advisory group for Institute for Healthcare Improvement (IHI’s) Age-Friendly Health Systems. At its core, an Age-Friendly Health System looks to optimize value for your loved one, the family, caregivers, and the healthcare system. An Age-Friendly Health System is looking for a win-win solution for everyone involved. Dr. Tinetti identifies the keys to providing the best care possible for older adults.
As individuals age, they amass more clinical conditions that become more complex over time. Seniors are individuals and it is important to remember each person’s outcomes, values, and desires are unique; they cannot be generalized. The healthcare team must recognize this individuality, and respond to the person’s specific needs, interests and priorities. When providers generalize or don’t take into account the variability of seniors, then there may be unintended care consequences.
The 4Ms
The “4Ms” is a part of an age-friendly approach focusing on improving the care that is complex and helping to make it more manageable. Regardless of the condition, the number of functional issues, culture, ethnicity or religious background, the “4Ms” are applicable.
- What Matters — Acknowledges that older adults vary in what matters most to them about their health, and their health care
- Medication – The number, types, availability/access, tolerance
- Mentation — Mental activity. This includes the “three Ds” of the 4Ms (depression, dementia, and delirium)
- Mobility – How well is the individual able to get around
It is important for clinicians to examine each of these areas (What Matters, Medication, Mentation, and Mobility) collectively for each individual at every interaction.
Caregiver Implications
These “4Ms” are intricate issues that are related to each other. They provide insight into some of the challenges associated with managing complex conditions. Common chronic conditions include Parkinson’s, dementia, diabetes, heart failure, and renal disease. When multiple serious chronic conditions coexist, the intricacies of clinical management become more challenging. It is important to remember that each individual is unique, and each person responds in their own special way.
Share with your provider
- What’s important to you from a health perspective, how you “like” to live, needs, what you value, and your Advance Directive wishes
- All medications that are taken; including over the counter, vitamins, supplements, creams, and prescriptions from other providers. Do not assume that one provider has a complete list of all the medications that are being taken
- Feelings, being sad, “feeling blue”, forgetfulness and any strange new or unusual emotions
- Any changes in the ability to “move”, includes changes in walking, being able to get out of bed, chair or tub, climb stairs, change in range of motion or ability to pick up items
Individuals and caregivers should remember the IHI’s Ask Me 3: Good Questions for Your Good Health that should be asked during each provider visit.
- What is my main problem?
- What do I need to do?
- Why is it important for me to do this?
The Ask Me 3 questions help you to focus on the important issues that are affecting your condition at a particular time. These questions become a nice introduction to the “4Ms” that providers are beginning to utilize in care management. You are encouraged to use the “4M” as a means of reminding the provider of your “uniqueness,” and desire for the best possible care. Open the provider discussion to the “4Ms” if the provider has not done so, as they tie in nicely with any treatment, or medication change made. These questions and approach encourage and assist in improving communication with the provider. They are a framework for better understanding of the proposed treatment or medication.
Insensitivity to Caregivers Stings

Caregiving is often a 24/7 role, and as the loved one declines the caregiving responsibilities increase. The physical and emotional toll of watching a loved one decline coupled with the increase in caregiving demands, lack of sleep, change in routine, and added responsibilities can result in a very stressed caregiver with fragile emotions. Some caregivers experience “role reversal”; activities and responsibilities that were once performed by the loved one now fall to the caregiver to address, in addition to all the other caregiving duties. There are many individuals who have never cared for a chronically ill person or a loved one who is experiencing memory loss, thus increasing physical limitations and have no appreciation for what goes into caregiving.
The Caregiving Reality
For many, caregiving activities involve some degree of bathing, toileting, grooming, feeding, assisting with walking or moving into a chair, meal preparation, medication administration, dressing changes, therapies, and keeping the loved one safe. In the event that the loved one does not sleep or requires assistance with repositioning, toileting or medications at night, that results in the caregiver is not getting sufficient rest, therefore, putting their health at risk. Beyond the physical activities associated with caregiving, the caregiver still must keep the household going. Additionally, the tasks of shopping, laundry, bill paying, house cleaning and maintenance, and potentially working, can all represent functions that caregivers must address and worry about.
The “Comments”
Although friends and family are well-meaning, they don’t always have a behind the scenes appreciation for what the caregiver is doing or experiencing. It is important to realize that remarks or questions can be interpreted by the caregiver as inappropriate, rude, demeaning, stupid, devaluing or insensitive. When stressed caregivers are tired and frustrated, they often experience heightened sensitivity to criticism. Individuals who do not know what to say, or don’t think through the implications of their remarks are unaware of the lasting impact of what they have said to a caregiver.
Particularly stinging are comments relating to the mood of the caregiver such as “cheer-up”, “Why are you struggling?”, “you look tired/worn out”, “you should not have to provide the care”, “put your loved one in a facility”, “your loved one does not even know/appreciate what you are doing for them” depict the type of comments that leave caregivers upset and frustrated.
To be supportive of caregivers
- Acknowledge what they are doing
- Acknowledge that the role is stressful
- Make a reference to something they are doing that is making a difference for a loved one
- Offer words of encouragement such as:
- What you are doing is important
- You are making a difference for your loved one
- Your loved one is lucky to have you
- You have a very special relationship with your loved one
- I admire what you are doing
- I support the effort you are making for your loved one
- I would be honored/lucky to be cared for like you are doing
- Listen
- Smile & give a hug
- Offer specific assistance – Bring a meal, do a chore, run an errand to lighten the load of the caregiver
Avoid
- Making judgements about their caregiving role
- Criticizing what they are doing
- Talking down or treat the caregiver or loved one as a child
- Making the conversation about the non-caregiver and their experiences
- Referencing a future reward for their caregiving responsibilities
- Comparing caregiving experiences, each is unique yet there are commonalities
Consequently, caregivers who are at the receiving end of insensitive remarks have the choice as to how they respond. There may be times that ignoring or not responding to the comment is best, hence the individual runs the risk of focusing or dwelling on the insensitive remark and having it impact the relationship. Responding calmly is an art. Sharing that the comment was hurtful or insensitive, along with the feeling evoked may help avoid future hurtful comments. There may be individuals the caregiver wants to engage in addressing the specifics of a comment that could result in brainstorming or specific requests for assistance and support.
If you know a caregiver, go out of your way to do something special for them, lighten the burden that they are carrying. You will both feel better after your act of kindness has been received. Check out Home Hospice Navigation: The Caregivers Guide for additional suggestions and resources.
End of Year Personal Report Card
As the year draws to an end, this is a time to review the year from a variety of perspectives. Often, an individual’s financial health is the one area that gets the most focus. Evaluating the status of investments, retirement contributions and making last-minute donations to charitable organizations are the top areas of attention. Some individuals take advantage of funds left in their Flexible Spending Account (FSA) and get needed dental work, glasses or other medical services that have been delayed.

Financial health, and physical assessments and treatments, are not the only areas to address. A key area is a review of your Advance Directive paperwork, this is crucial for individuals of all ages as serious accidents or illness can occur at any time of life. Consider:
- Do you have an Advance Directive?
- Does your Living Will reflect your current wishes?
- Have you had a health crisis since outlining your wishes and your forms need modifications?
- Are your choices of Healthcare Surrogate and Financial Power of Attorney still appropriate?
- Are those individuals still able to carry out your wishes?
- Are any home modifications needed to remain safe, and age in place?
- Do you need to purchase Long Term Care Insurance?
- Do you need to self-fund for long term care needs?
- Is your Last Will & Testament up to date and reflect your current wishes?
Resources for Advance Directives include The Five Wishes, Death Over Dinner and The Conversation Project. The holidays are a great time to share your wishes with family, allay their concerns and address any questions that surface. Having your family around to hear from you directly what your end-of-life wishes are, and how you want to be cared for when you are unable to share your care wishes, is a gift. It often is a very hard gift to share, due to the emotions associated with recognizing that you are sharing how you want to live while dying. Once shared, you will experience peace of mind and know if there are any issues between family members that need to be resolved.
Check out Home HospiceNavigation: The Caregiver’s Guide for additional information. Free resources and links available at www.JudithSands.com
Thanksgiving has become the time to show appreciation and celebration of family, health and good fortune. Expressing gratitude when caregiving, can be very challenging, especially as a loved one is declining physically and mentally. Too often we become focused on what has been lost physically, mentally and emotionally; that we fail to recognize that there are still things that we should be thankful and grateful for. Being grateful refocuses us, on the positives we encounter. At times we fail to recognize the simple gestures extended to us, it may be a friend who calls or sends regular greeting cards, someone who brings a meal or assists with a chore or task that we are unable to perform. The acts of “goodness” and kindness, expressed towards us are humbling; they stop us forcing us to acknowledge that we have “forgotten” to appreciate the goodness around us. On this Thanksgiving take the opportunity to reflect on all that is good and kind around you, reach out to someone, return the kindness and acknowledge them for what they mean or do for you. May this be a time of blessings for you and your loved one.

November is known as Palliative Care & Hospice Care month. A time to recognize the professionals dedicated to symptom management and end-of-life care. This is also an important time for individuals of all ages to discuss their end-of-life preferences and wishes with loved ones and their physician. Take the time to complete or update Advance Directive forms. Consider sharing these preferences at Thanksgiving with family and friends, providing the opportunity to stress your desires and address concerns.
Resources to assist you in the discussion process include Conversation Starter Kit a resource that is available in multiple languages, includes a version for those with Alzheimer’s/dementia and those with a seriously ill child. These resources are from the Institute for Healthcare Improvement (IHI). Another valuable resource is Death Over Dinner that helps you plan a dinner party to articulate end-of-life preferences. “The dinner table is the most forgiving place for difficult conversation. The ritual of breaking bread creates warmth and connection, and puts us in touch with our humanity.” The site has a number of versions including an Australian, Jewish and Brazilian edition.
#deathdinners #palliativecare #palliative #hpm #homehealth #compassion #caregiving #familycaregiver #joyincaregiving #hospicecaregiving #caregivertips #caringforfamily #HomeHospiceNavigation #HomeHospiceCaregiving #HomeCare #VNAA #IHI #DeathOverDinner
Coming to the realization that additional caregiving assistance is needed may be obvious to some and very challenging for others to realize. The need for more caregiving support affirms that the current caregiving plan is not meeting the changing needs of the care recipient. Some view this need for additional assistance as a very difficult and painful realization that they are not able to fulfill all the care needs of the loved one.
How to find a caregiver? Just like dating, ask for a referral from a trusted friend, colleague, spiritual advisor and anyone you come in contact with. Caregivers are typically not free, so be sure you have a realistic budget and recognize that as an individual declines, usually additional caregiving hours are needed. There are “dating services” also known as non-medical homecare agencies and registries to assist in the caregiver identification process. Be sure to ask about the background checks and screening processes used. No matter how you find the “professional” caregiver, they need to be the “right” match for the care recipient and the circle-of-care at the bedside. Whenever possible, speak directly with someone who has hired this individual to gain first-hand insight about them and their abilities.

Try to meet the individual prior to the initial caregiving session if possible. This is the time to determine if the potential caregiver is the “right fit” for the care recipient. What is your “gut” reaction when you meet the individual? Do you have reservations or concerns? Consider, personality, temperament, willingness for the assignment, physical ability to meet and perform the care needs, availability to provide the hours needed (do they have other individuals for whom they provide care and you will need multiple individuals to cover the hours?) Can the caregiver easily communicate, and able to understand the wishes of the care recipient? Can the care recipient easily follow the instructions of the caregiver? Be sensitive to communication challenges. Are there cultural, ethnic or religious aspects that need to be clarified? If your loved one has special needs can the caregiver meet them? Does the care recipient have certain preferences, and can the caregiver abide by them?
As with dating, sometimes there is a mismatch, be sure to have an exit strategy with a corresponding back up plan. Sometimes “blind dates” work, and other times they do not. Be realistic in your expectations, address what is important to you and the care recipient and also take the time to learn about the caregiver, establish guidelines and expectations up front and together to ensure minimal disruptions to the care recipient.
Financial implications associated with hiring a caregiver will be discussed in a future post.
#palliativecare, #palliative, #hpm, #homehealth, #compassion, #eol, #caregiving
The fitness for caregiving duty question should not be taken lightly. Is the caregiver Willing, Able & Available needs to be asked and responses evaluated continuously during the caregiving journey ensuring the caregiver ability to meet the demands of the role, and that the loved one’s care needs are being safely met. Typically, when a loved one has physical or mental status change there will be a corresponding change in caregiving needs. As the loved one’s condition declines, the care needs typically increase. The additional care requirements mean more frequent and complex caregiving interactions that can be emotionally and physically draining. Caregiving assistance that may have been periodic or supportive in nature shifts to being more intensive. Intensive caregiving requirements go beyond some assistance with bathing and grooming, toileting, feeding, dressing, transferring and walking to having to meet all of those needs with extra assistance. This corresponds to spending more time and energy on the various caregiving functions while continuing to manage medications and keeping the loved one comfortable.

The questions that caregivers and their support system need to continuously evaluate are:
- Is the caregiver able to meet the care needs of the loved one? That is, can they physically and mentally complete the caregiving tasks safely? If the recipient of care is physically taller and heavier than the caregiver there will be physical constraints, including limitations in the ability to lift, turn, safely walk and provide the assistance with activities of daily living. Is the caregiver able to cope with the demands of caregiving?
- Is the caregiver willing to meet the care needs of the loved one? That is, does the caregiver feel comfortable and willing to assume these additional tasks that may include emptying bedpans, dealing with vomit, handling additional bodily fluids, managing medical equipment and supplies?
- Is the caregiver available to meet the care needs of the loved one? That is, can the caregiver be present to carry out the necessary care? Does the caregiver have conflicting responsibilities such as work, child care or other obligations that will impact their ability to meet the needs of the loved one?
If the answers to these questions is “no” that is a clear indication that additional caregiving support is needed. This is the time that the members of the circle-of-care, needs to reevaluate the caregiving plan and make modifications to meet the recipient’s needs.
Don’t forget that caregivers need to opportunity to “recharge” and take care of their own physical and emotional needs before meeting the needs of others. Friends of caregivers need to help the caregiver get the required time away for a bit of relaxation, a tasty meal, run an errand or read a book. Remind the caregiver of the instructions given on a plane, that when the oxygen masks come down, always put on your own mask before assisting others. Evaluate your caregiver situation for being able, willing and available to perform the needed care tasks.
#palliativecare, #palliative, #hpm, #homehealth, #compassion
Don’t delay, order your copy of
Home Hospice Navigation: The Caregiver’s Guide today!





